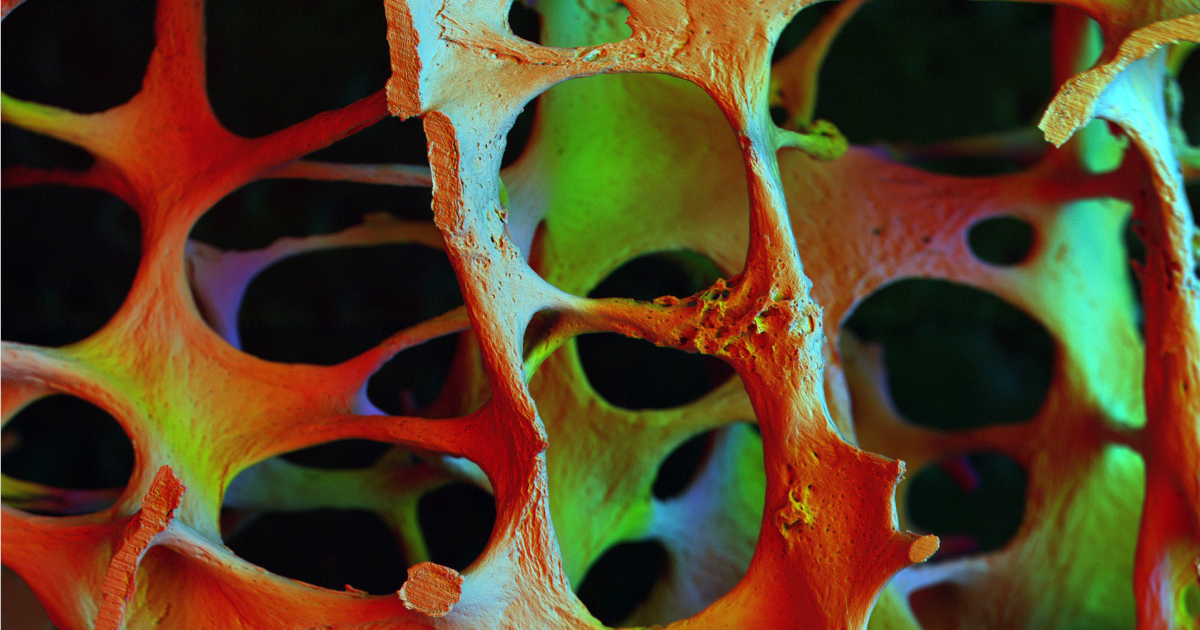
We will achieve this mission by optimising musculoskeletal health (bone, muscle and joint) through the development and testing of lifestyle, behavioural and pharmacological interventions informed by our observational studies; and by using these findings to influence health policy.

Our specific aims are to:
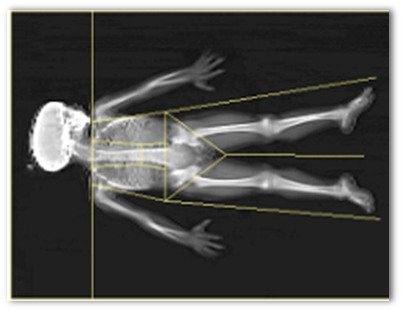
- delineate the environmental influences, throughout the lifecourse, of age-related musculoskeletal (osteoporosis, osteoarthritis and sarcopenia) and metabolic disease;
- use our findings to develop and test population-based and targeted interventions to improve musculoskeletal and metabolic health throughout the lifecourse;
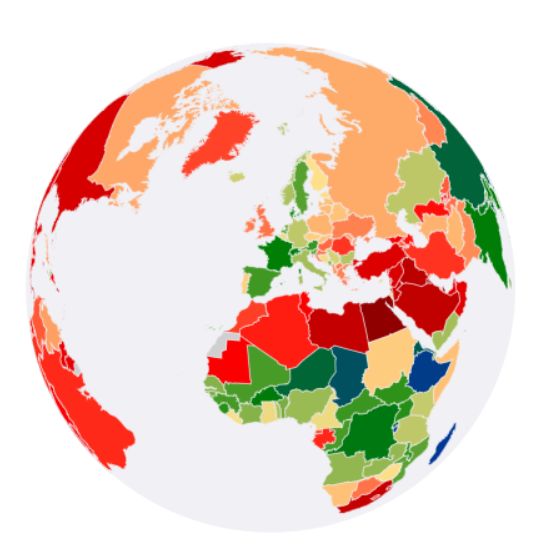
- maintain and develop the long-term cohorts/trials assembled in Southampton as national and international resources to explore the mechanisms underlying the developmental origins and later causes of musculoskeletal health and disease;
- inform health policy and promote training, research capacity development, knowledge transfer and public engagement in lifecourse epidemiology.

The purpose of our research is to elucidate important, preventable causes of these common non-communicable musculoskeletal disorders and their complications. Through an understanding of the causes of these disorders, and the development and evaluation of interventions at appropriate stages in the lifecourse, we aim to provide robust and timely evidence which informs policies to improve population and individual health.
Musculoskeletal disorders constitute a major public health problem: the Global Burden of Disease study estimates that the category imposes the second highest impact on years of life lived with disability, and is set to rise by over 40% by 2050.1 The costs associated with these conditions are equivalent to 3% of gross national product each year. Indeed osteoporosis and osteoarthritis (the most common metabolic bone and joint disorders respectively) account for 6.8% of total disability with a remaining lifetime risk of osteoporotic fractures at the hip, wrist or spine of 39% among women and 13% among men at age 50 years;2 the annual NHS cost of managing osteoporotic fractures is £4.2 billion, half of which is attributable to hip fracture.1 From age 50 years, lifetime risks of total knee arthroplasty (representing end-stage osteoarthritis) are 10.8% for women and 8.1% for men.3 Sarcopenia, the commonest muscle disorder worldwide, is estimated to cost £2.2 billion in the UK each year.4
- Harvey NC, Curtis EM, Dennison EM, Cooper C. The epidemiology of osteoporotic fractures. In: Bilezikian J, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 9th ed. Hoboken NJ: Wiley; 2018. p. 398-404.
- Holroyd C, Dennison E, Cooper C. Epidemiology and classification of osteoporosis. In: Hochberg MC, Gravallese EM, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, editors. Rheumatology. 7th ed. Philadelphia PA: Elsevier; 2019.
- Bruyere O, Cooper C, Arden N, Branco J, Brandi ML, Herrero-Beaumont G, Berenbaum F, Dennison E, Devogelaer JP, Hochberg M, Kanis J, Laslop A, et al. Can we identify patients with high risk of osteoarthritis progression who will respond to treatment? A focus on epidemiology and phenotype of osteoarthritis. Drugs Aging. 2015;32(3):179-87.
- Dodds RM, Roberts HC, Cooper C, Sayer AA. The epidemiology of sarcopenia. J Clin Densitom. 2015;18(4):461-6.
Research
Promote human health using lifecourse epidemiological methods

Cohorts
Studies related to generational cohorts across the lifecourse
Training
Learn high quality population health science with us