The potential of tissue engineering.
I find the potential of tissue engineering to be very interesting, mainly because I believe that there is no limit to the potential. One of the main uses for tissue engineering is to replace lost tissue and to maintain damaged tissue or even potentially an entire organ. But that is another issue altogether!
There are some other aspects to tissue engineering, and these include regenerative medicine, which has been used interchangeably with tissue medicine.
The interesting history of tissue engineering
The idea of tissue engineering has always been more of a dream or a fantasy before modern technology came about. A very intriguing perspective that I have found recently explores the idea that the concept of tissue engineering has been around in the early history of man, which is the story of Eve being created from the rib of Adam. This is so fascinating to me because it shows how humanity has this innate desire to create and not be bound by any limitations.
However, in modern times, the concept of tissue engineering was introduced in the late 1980s, and this opened a gate of endless possibilities and different applications for the future.
One of the first examples of tissue engineering being successfully implemented was in 1991, when an individual with Poland’s syndrome was the first human to receive a tissue-engineered implant that was composed of synthetic polymer.
The ability to save human lives.
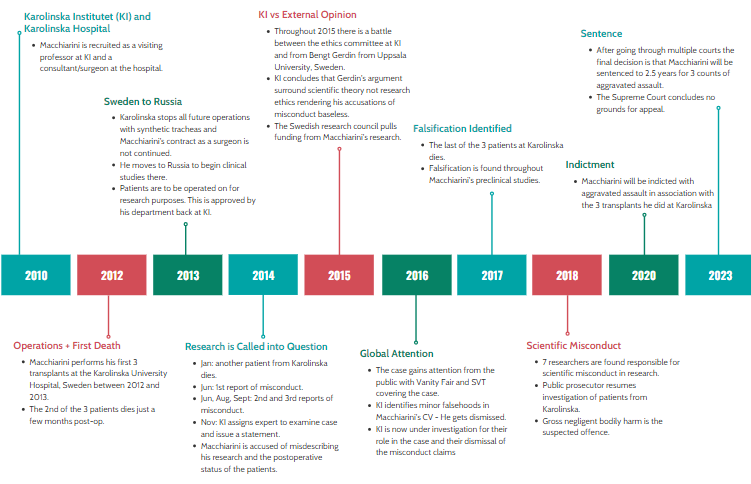
Unfortunately, in our world currently, there is a shortage of organs that are available for transplantation. Additionally, I was saddened to find an article in the New York Post showing how there are failures in the management of organs and a lot of available organs are actually going to waste and will be discarded even though the number of people that are in desperate need for a new organ will never run out. It was reported that around 17 people die per day while waiting for a transplant, and there are around 106,000 people in America on the waiting list.
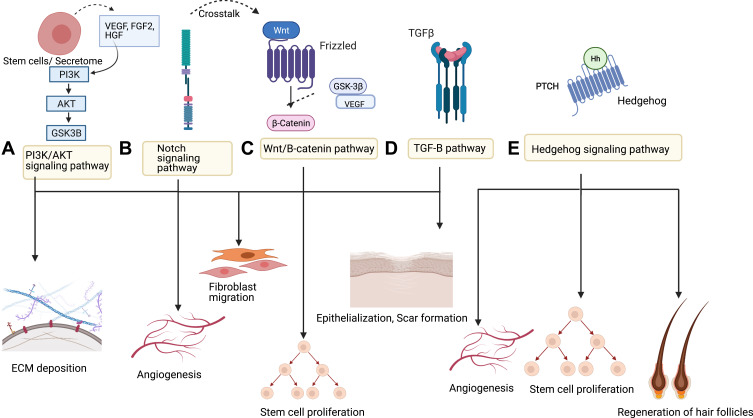
This is why I believe that tissue engineering can provide a possible solution to this devastating problem. With the improving technology, the possibility of creating 3D organs is increasing, with biomedical engineering researchers developing 3D temporary organ structures called scaffolds. With this technology, the possibility of creating material that can help with recovery is increasing.
Problems with Tissue Engineering
I am very excited about the prospect of tissue engineering and its potential future applications. I am very aware that there are limitations to this.
Some of these limitations are the materials used. For example, alginate is a difficult material to use as it collapses easily. Moreover, the challenge I believe to be the hardest to overcome is receiving donations from others.
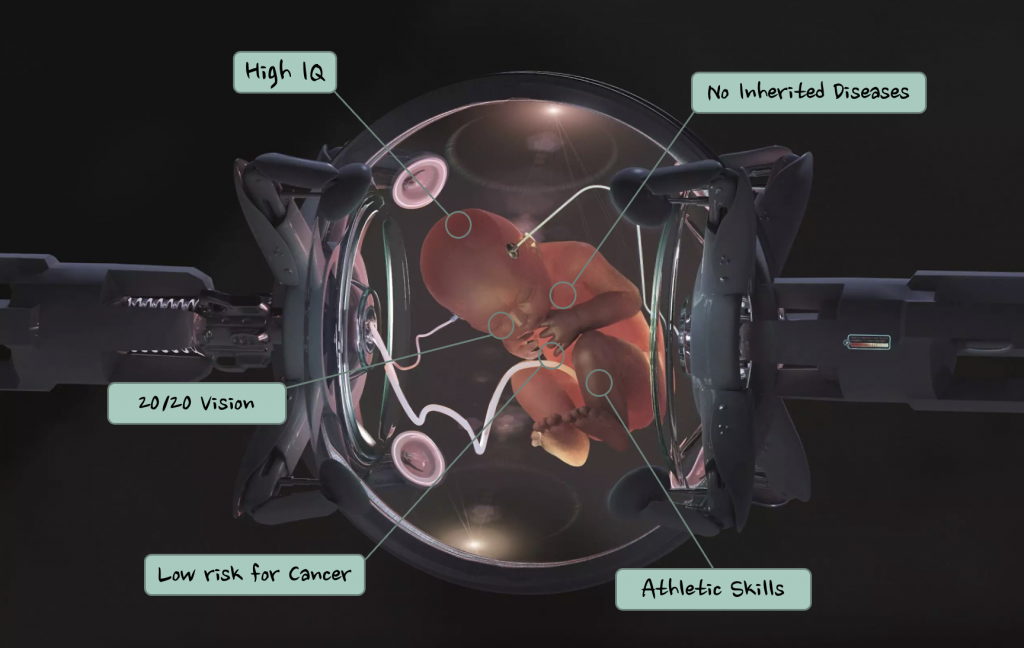
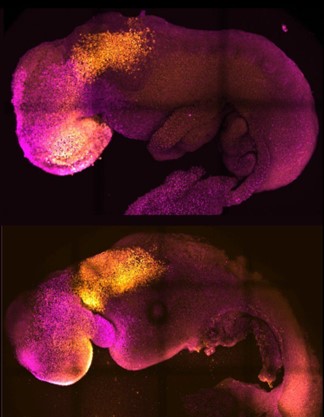
If we were to use stem cells to engineer tissue for another, there are many ethical questions that must be addressed, such as the problems of taking stem cells from a human embryo.
In my humble opinion, I believe that taking stem cells from an embryo is unethical, and this mainly revolves around religious problems, as being raised in a catholic family has shaped my views on certain matters such as this.
However, if improved communication to try and get more people to donate their stem cells, then it may be possible to overcome this problem, and many more lives could be saved in the future.







Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…