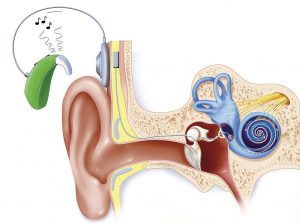
NICE guidelines state that ‘simultaneous bilateral cochlear implantation is recommended as an option for […]: children; adults who are blind or who have other disabilities’. Unilateral cochlear implantation is recommended for those with severe to profound deafness but bilateral cochlear implantation is not recommended on a cost-effectiveness basis. With the improvements shown below for adults after receiving a second implant, why does the NHS only cover unilateral implantation?
| For Bilateral Cochlear Implants | Against Bilateral Cochlear Implants |
| Improved speech perception in noisy situations | Possible worsening of tinnitus as a side effect |
| Improved directional perception of sound | Not considered cost-effective |
| Easier, less exhausting conversation |
When making decisions for the guidance ‘the committee did not consider […] different cochlear implant systems were associated with different cost-effectiveness profiles’. The main focus of the guidelines was to find the cheapest option to restore hearing, and this is repeated throughout the document. The guidelines were made in 2009. A 2018 update included a 15% reduction in costs that were not adjusted for in cost-effectiveness profiles, and a lack of update as to current models on the market.
It was found that for a simultaneous bilateral implant in an adult to be cost-effective, the NHS would require a 75% discount on the second implant. Although simultaneous bilateral implantation has better results than sequential bilateral implantation, adult patients who wish to have bilateral implants are forced into sequential implantation as they must fund the second implant themselves.
It is time these guidelines are reassessed using a larger sample size and a greater focus on patient wellbeing and quality of life. If data still shows that bilateral implantation is not cost-effective, could the NHS look to cover some of the second implant cost?
Deaf adults should receive the same level of care as deaf children. The data used is identical for children and adults, but the NICE committee came to the conclusion that children are more cost-effective and will have a greater improvement in quality of life after receiving bilateral implants. Expecting deaf adults to pay upwards of £20,000 for their healthcare when other, more expensive surgeries are covered does not sit right with me. This leaves deaf adults unnecessarily struggling day to day which is unfortunate given people with hearing loss are twice as likely to experience mental health difficulties.
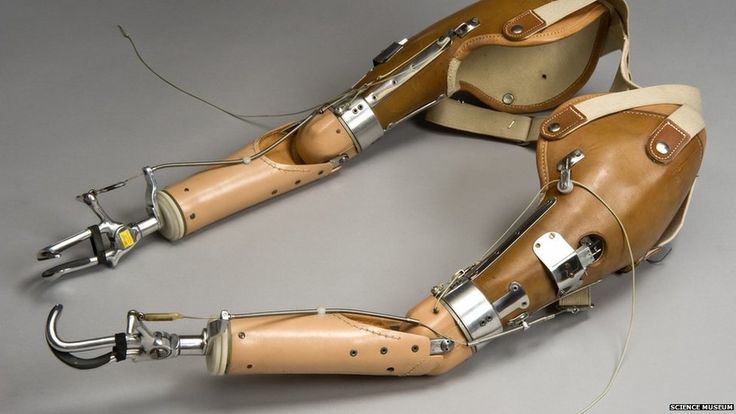
Making the only route to restoring hearing to the level science can an expensive one is unfair to put on someone who is likely to be struggling to work. This is particularly prominent for those with sudden deafness (i.e. from illness or injury) or those whose hearing has declined rapidly, preventing them from having time to save money. Many people end up fundraising for their second implant, but restoring hearing should not be a luxury few can afford – particularly given that the individual cost of an expensive implant is not far below that of a pair of cheaper implants.









Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…