My Experience with Implants
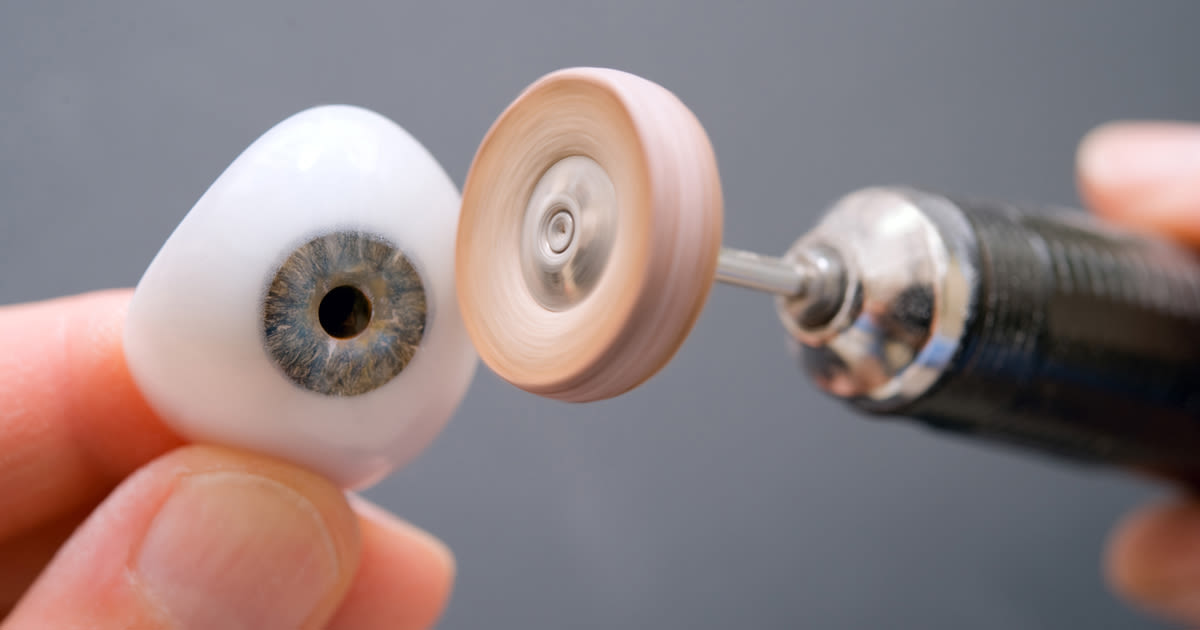
What’s every teenager’s worst nightmare? To me, it was being told at the young age of 13 that I was missing 2 adult teeth! But why was this such a bad thing? Because the corresponding milk teeth would eventually become too weak, fall out, and nothing would grow back. 9 years later brings us to now, and unfortunately, that dreaded day came. Luckily for me, the medical world has advanced, and dental implants exist, meaning I don’t have to be ‘toothless forever’, or so I thought.
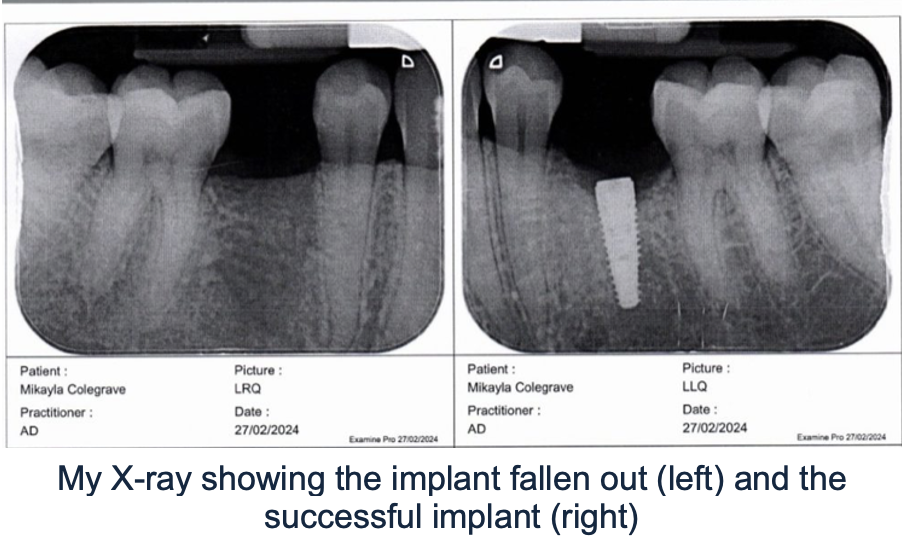
Recently, 1 out of my 2 implant screws decided it was going to fail and fall out causing a delay in receiving my new teeth. I felt this massively inconvenienced me as I now must remain ‘toothless’ for a little longer. However, this experience had me thinking about the bigger picture of implant failure and I realised that my implants were only for cosmetic purposes. What if my implant was for my knee or hip and that was to fail? How much of an inconvenience would that be? Intrigued, I decided to dive deeper into the topic.
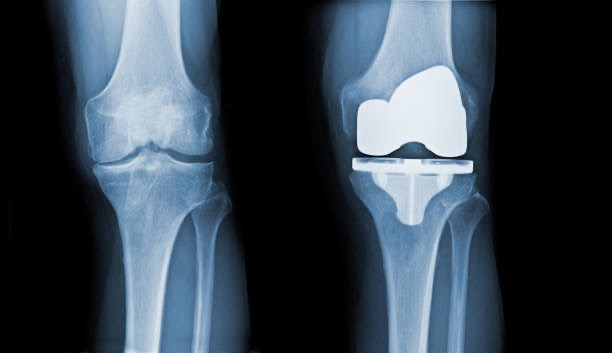
Implant Failure in Joint Replacements
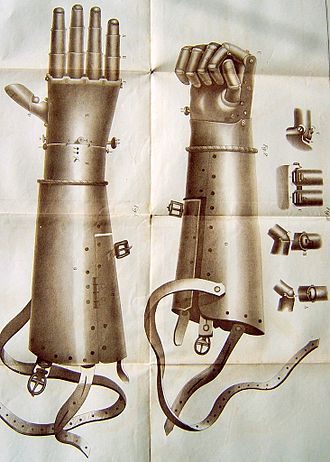
From reading this article by Steven Richard Knight et al, I’ve learnt that, amazingly, hip replacements date back to over 100 years ago when the first surgery took place in 1891 in Germany. Ever since then total joint replacement has advanced in the materials being used, the surgical techniques and technology. This has helped with the life expectancy of the implants which ultimately has reduced the percentage of failure seen today. Although it’s not foolproof yet.
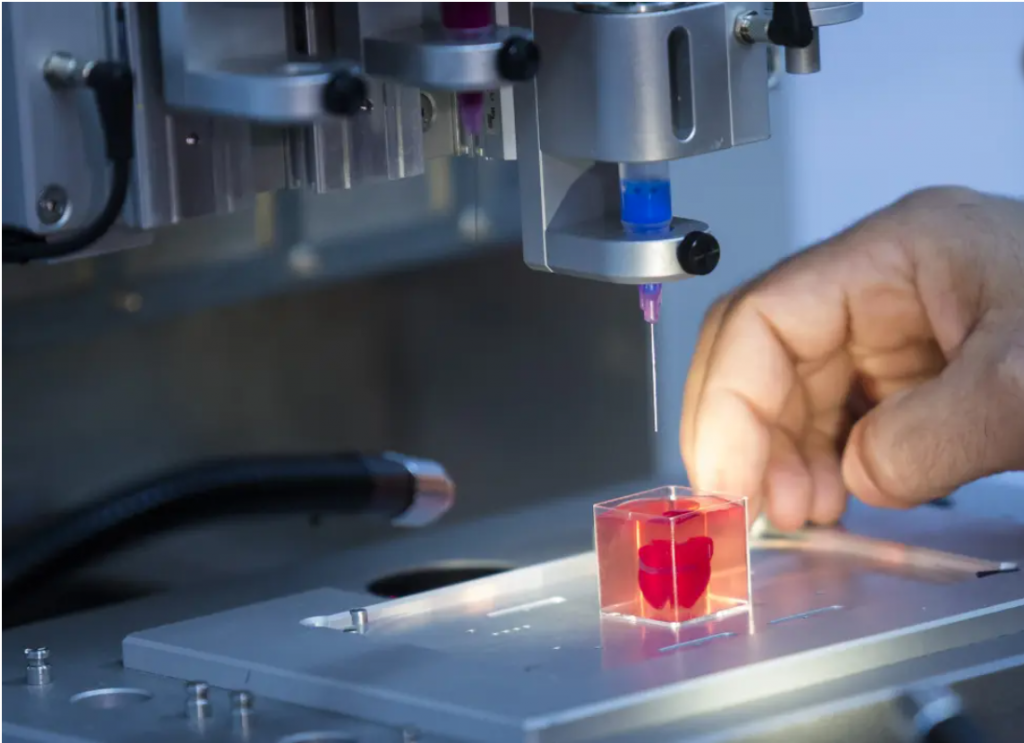
Joint replacements are mostly seen in people over 60 due to factors such as osteoarthritis. However, they aren’t uncommon in the younger generation. In a study by Lee E Bayliss et al, I found it interesting that you are more likely to experience implant failure if you’re younger. After further reading, I started to understand why this is the case. Imagine living a day in the life of a 20-year-old and then a day as an 80-year-old. I’m sure you will agree that these days are substantially different. At 20, you’re going to be more active which causes the implant to be put under more strain. This causes the bone to wear down causing it to loosen and fail. However, aseptic loosening isn’t the only reason for implant failure. Other factors such as infection can also be a cause which you can find out more about here.
The Complications of Major Implant Failure and How it is Resolved
When my implant was failing it was obvious to detect as it started to rise out of my gum until it eventually fell out. However, I began to wonder how you would be able to tell if an implant placed inside your bone was failing. I did some research on the symptoms and it explained how you would experience severe pain and instability in that joint. Imagining what that would be like I decided that although I felt very inconvenienced, it was minor compared to this. These patients would have to endure 1-2 more surgeries to receive joint revision and I only have to wait for the bone to heal before replacing my dental screw. However, even though implants come with a risk of failure, I think it’s incredible that doctors can fix these problems and I think it’s a risk worth taking.

















Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…