
Modern advancements in technology have given humans the capability to utilise the body in ways that were never even considered as being possible 100 years ago. As a Biomedical Electronics Engineer, I’m passionate about the application of myoelectric prosthetics to help people achieve a better quality of life – something made possible through modern engineering marvels.
My passion for this stemmed from a BBC show named “The Big Life Fix”, in particular, an episode about a girl who wanted to become a dancer but was unable to do so due to a partial leg amputation. The engineers on this show designed her a custom prosthetic which allowed her to fulfil her dream – this inspired me and made me want to follow in their footsteps.
The lecture about biological sensing particularly appealed to me, especially the article written about the “bionic arm powered by AI”. This article demonstrated how a man, born with no lower arms or legs, was shocked at the research and development made by a company in California. This prosthetic combined EMG with machine learning to power a prosthetic arm capable of performing many complex movements, whilst also having haptic feedback which allowed the user to feel when they’re gripping something. The combination of these technologies made me question: What other technologies are used in prosthetics?
What other technological innovations are evident in the prosthetics industry?
Further exploration into this showed that many modern prosthetics use machine learning to improve their efficiency. Machine learning is a form of AI which relies on complex algorithms to analyse data and “learn” which data is more favourable, leading to more human-like decisions. Combining this with electromyography (EMG) and electronic systems paves the way for the potential for the creation of life-like artificial limbs.
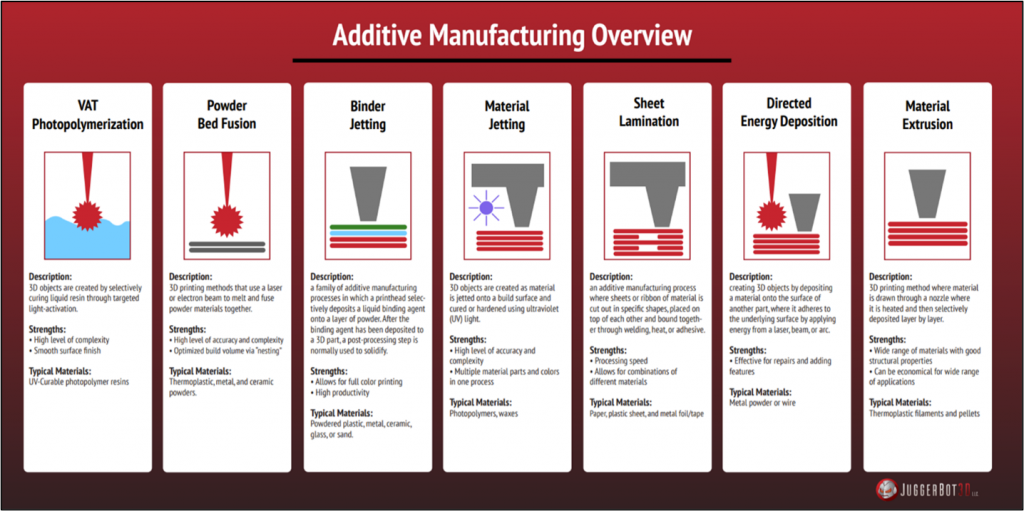
Whilst 3D printing does not contribute significantly to how a prosthetic is powered, modern advancements in these technologies have allowed for rapid prototyping. The different methodologies, varying from FDM (Fusion Deposition Modelling) to SLA (Stereolithography), alongside material innovations have lead to a conclusion that 3D printing is an entirely suitable manufacturing process for prosthetic production, especially as the lead times can be very short.
Ethical Issues with Prosthetics
Whilst the idea of prosthetics is generally a positive topic, there are issues regarding their sustainable use. A study by researchers at the University of Bristol suggests that humans could become overdependent on embodied devices which results from the seamless inclusion of machine learning. An argument that they made was that a prosthetic user would be unable to act effectively in an emergency situation due to the slow and sometimes inaccurate feedback of the device.
Another factor to consider is that some prosthetics can be invasive, requiring sub-surface EMG electrodes, with others requiring friction-fit sleeves which, over time, could cause injury to patients adding further financial stress to the healthcare sector.
Assuming that ethical issues are taken into consideration and legislation is followed, prosthetics could become the forefront of future limb rehabilitation.
The combination of these technologies with new innovations and improvements is improving the quality of life of countless individuals, which I find truly inspiring. Technology has improved drastically within the last 100 years, so the true capabilities are really unknown. Potential issues today could be solved in the near future – I find this very exciting, especially with the knowledge that people in the future requiring a prosthetic will have more promise and improved lives.


Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…