Background on Atom Limbs and Prosthetics

This is the first artificial human arm created by Atom Limbs called the ‘Atom Touch’.
Atom Limbs is a company whose goal is to build a better future for humans by building artificial prosthetics that allow amputees to regain function of lost limbs.

Prosthetics first emerged with the use of materials such as wood and metal, however current technology uses lighter and more durable materials such as carbon fiber and silicon. Despite the modern world having great advancements in technology, most prosthetic limbs have remained the same in that they give the appearance of a functioning limb but are relatively useless to the wearer.
Prosthetic toe from ancient Egypt
Ethical and Societal Considerations
Bionic products tend to be expensive which puts most devices out of reach for many disabled people, who statistics show are more likely to be on the poorer end of society. There may also be supply issues for low income countries who have limited access to specialised medical facilities. This seems to partially be why less than 1 in 5 people with arm loss do not use a prosthetic. So what is the point of making a device to improve quality of life if the intended target audience doesn’t use them?
I read this BBC News article and it appears that Atom Limbs have dwelled upon this ethical consideration positioning their bionic arm around £15,000, which – although still a lot – is considerably less than many other similar devices on the market. A more reasonable price for a high quality bionic product. This made me question myself – if I had a missing arm, would I get this bionic arm? Considering its price, my decision would come down to the prosthetics practicality and usability in everyday life. If it functions like a real arm, then it would be justifiable to spend such an amount as it is a life-long investment.
The Underlying Science
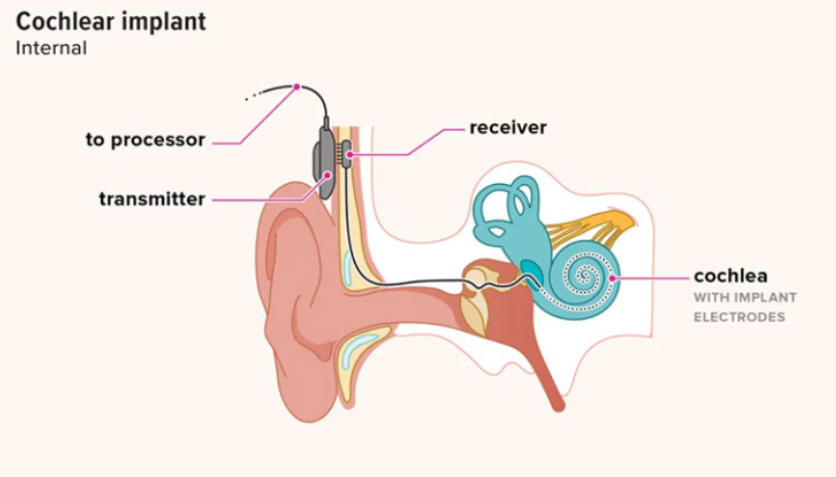
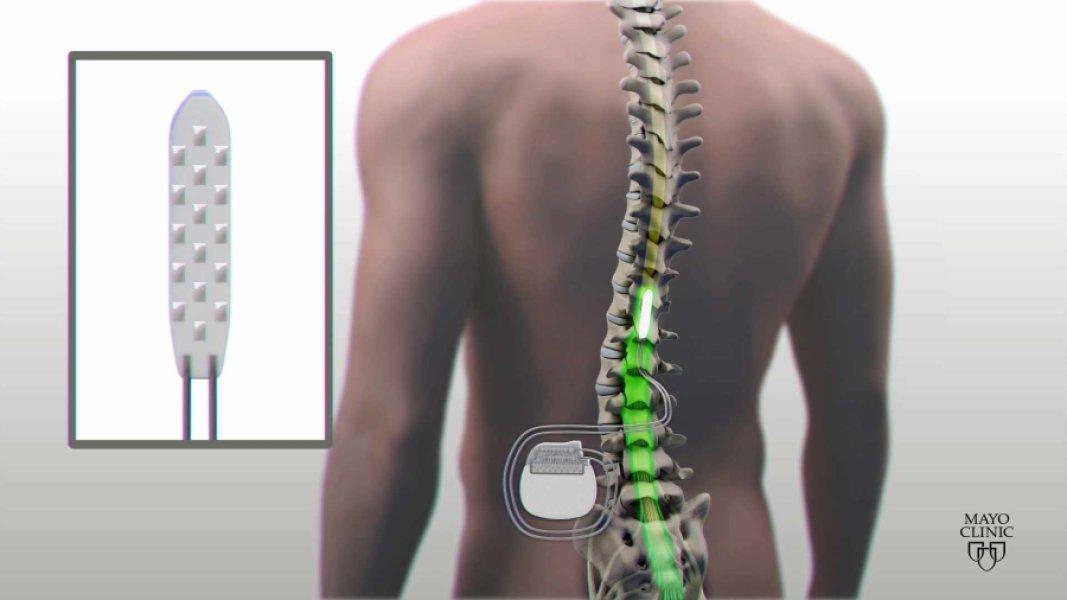
Neural Interface
Atom Limbs primarily relies on the use of advanced sensors and machine learning algorithms to interpret signals from the brain and utilise them to move a prosthetic limb. It connects to the wearer’s residual limb with bands of sensors that measure electrical signals produced from muscle movements. Signals are then picked up by electrodes and integrated. This innovative mechanism is known as myoelectric control.

Attachment
The arm attaches via a vest and is a non-invasive procedure which means no surgery is required for it to function. It uses breathable and lightweight materials providing comfort, which I believe would encourage amputees to choose the ‘Atom Touch’ over other prosthetic arms.
Haptic Feedback
One of the challenges posed in the use of bionic arms is the grip strength used on different objects. How would a wearer be able to tell how strongly they are gripping, for example, an egg to ensure it doesn’t crack? The answer is haptic feedback – this is delivered to the user through vibrations which are produced when sensors detect interaction with the environment.
Motion
The near-full range of motion in the elbow, wrist and individual fingers allows the wearer to fully interact with the world and regain their sense of touch. For someone who has not lost a limb, this may seem like a trivial feature, however for an amputee this may be an extraordinary feeling. An amputee reporter from the BBC News operated a digital version of the bionic arm.
“The notion of learning how to control a part of the body I don’t have is almost impossible to describe.”
Paul Carter from BBC News







Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…