Look younger, look natural, look flawless. In modern society, the pressure to reach an ever-more-unattainable level of youth and beauty as one ages is constant. There is a nonstop barrage of anti-ageing creams and pills advertised on TV and treatments and therapies available by estheticians and plastic surgeons. It all sends a clear message: ageing is offensive and ugly, and something to be prevented by all means possible, not embraced.
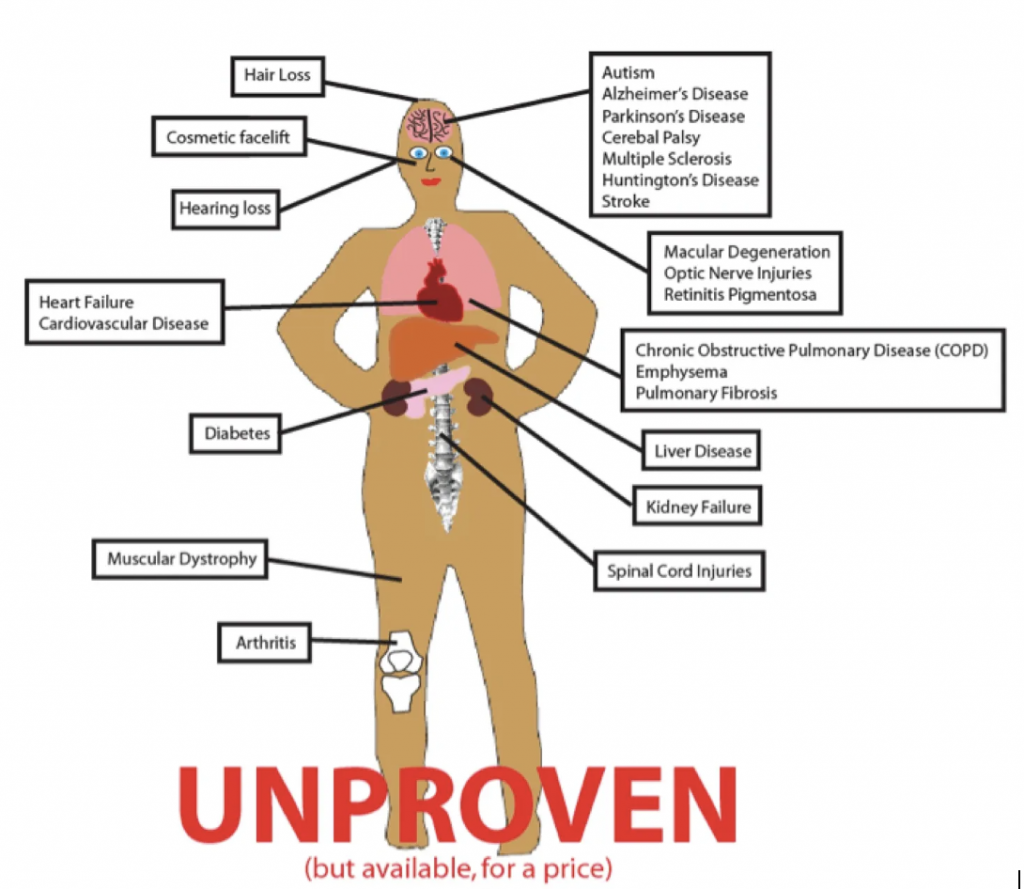
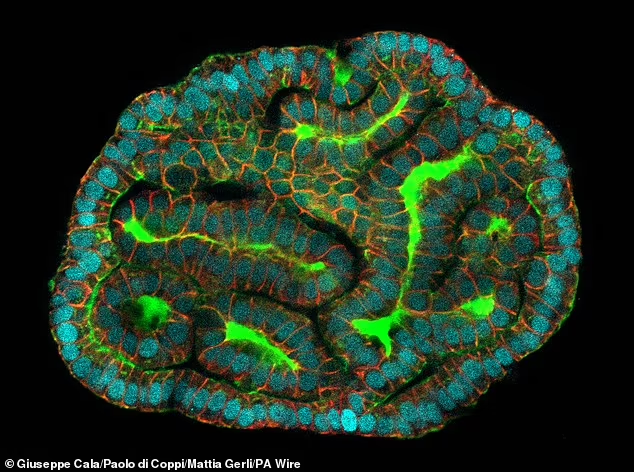
Another treatment joining the legion of other anti-ageing therapies is DermaGro—a ‘miracle’ stem cell technology that has been claimed to treat wounds and burns, relieve eczema, and reverse the visible signs of ageing. Unless you’ve been living under a rock, you’ve likely encountered the buzz around DermaGro. Its aggressive social media marketing and the heated debates about its efficacy and ethics have been hard to miss. Here’s a quick rundown on how DermaGro is purported to work:

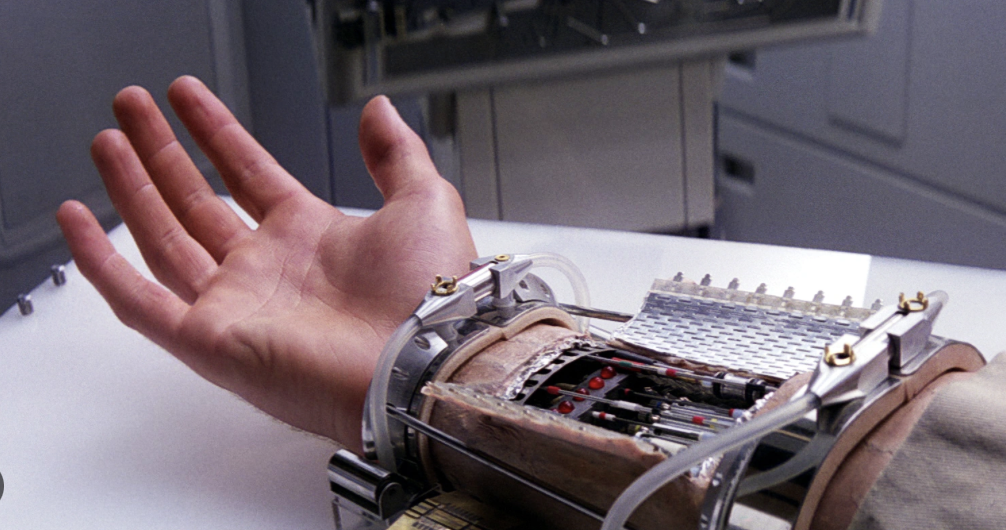
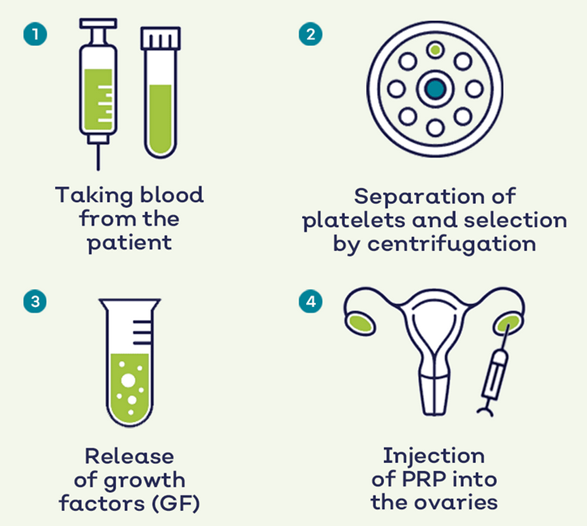
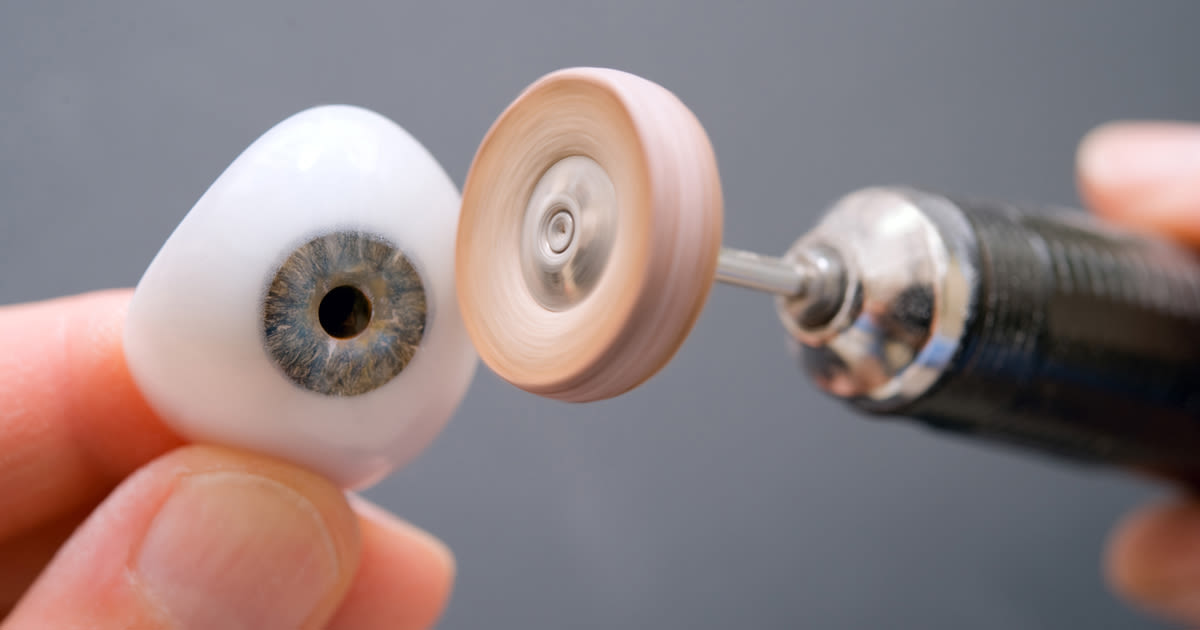
You sign up for their services online (and pay a hefty fee for the privilege), and soon after go to one of their clinics to have stem cell samples taken for culture. Once these are screened, selected, converted to selectively mutated and cultured, they are sent to you along with your starter kit (for yet another fee), followed by repeating deliveries of stem cells as and when you need them on a subscription basis (which if you haven’t guessed yet, comes with more fees and hidden charges!). You then keep your stem cells in the freezer until you need to apply them, which is done by loading them into the ‘gun’ and applying them to the wound. Easy enough right? They’re your own stem cells in your own home; how can there be any issues?
But there are issues aplenty… even if we ignore the ridiculous fees (you’re coming up to £3000 for just a month of treatment), there are still logistical issues. It is well known throughout stem cell research and bioscience in general that stem cells must be cryogenically preserved at -80 to below -150 degrees Celsius for them to be properly preserved and remain viable. However, DermaGro claims it is perfectly fine to store samples in a regular household freezer which only reaches temperatures of about -18 degrees Celcius, far too high for proper storage of stem cells.
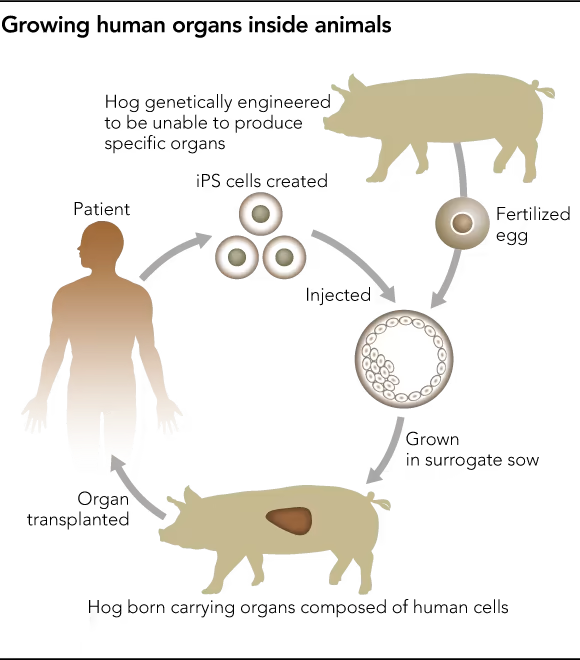
Additionally, DermaGro claims to offer a ‘donor service’ where another person’s allogenic stem cells are used as a replacement for the customer whose stem cells cannot be used. However, no one fully knows where these stem cells come from. Not even DermaGro’s CEO will answer the question when asked (I directly contacted DermaGro, the CEO’s personal email and asked via their Instagram stories to no avail). Although DermaGro implies otherwise, some people have theorised that they are excess cells taken non-consensually from other patient’s samples. This raises massive ethical issues as patients do not consent to their cells being used for other people’s treatments when they sign up, and they receive no compensation for assisting other people’s treatments. Another more theatrical theory is that, much like the Hwang affair, researchers within DermaGro labs and clinicians within their donation centres are being pressured to donate their tissue to increase the supply of allogeneic stem cells, although the proof for this is still yet to come to the surface.
Finally, and most damningly, there have been reports that some early DermaGro trial patients were given a cocktail of drugs to support their treatments, and upon the initial signs of the stem cells being rejected, immunosuppressants were added to the mix. This is absolutely absurd. It displays a deeply horrifying and frightening lack of medical duty and basic ethics by DermaGro. In what world is looking younger or healing a wound faster worth risking cancer? Ultimately, DermaGro is a scam—an expensive, immoral and dangerous scam at that and one which targets the superficial insecurities of ageing women. I certainly won’t let these predatory frauds ‘get under [my] skin’, but I hope this article will get under theirs. We’re now left with only one question: How long until someone dies from DermaGro?
Please note that this blog post is not for marking, and rather is a part of the group project assignment.






Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…