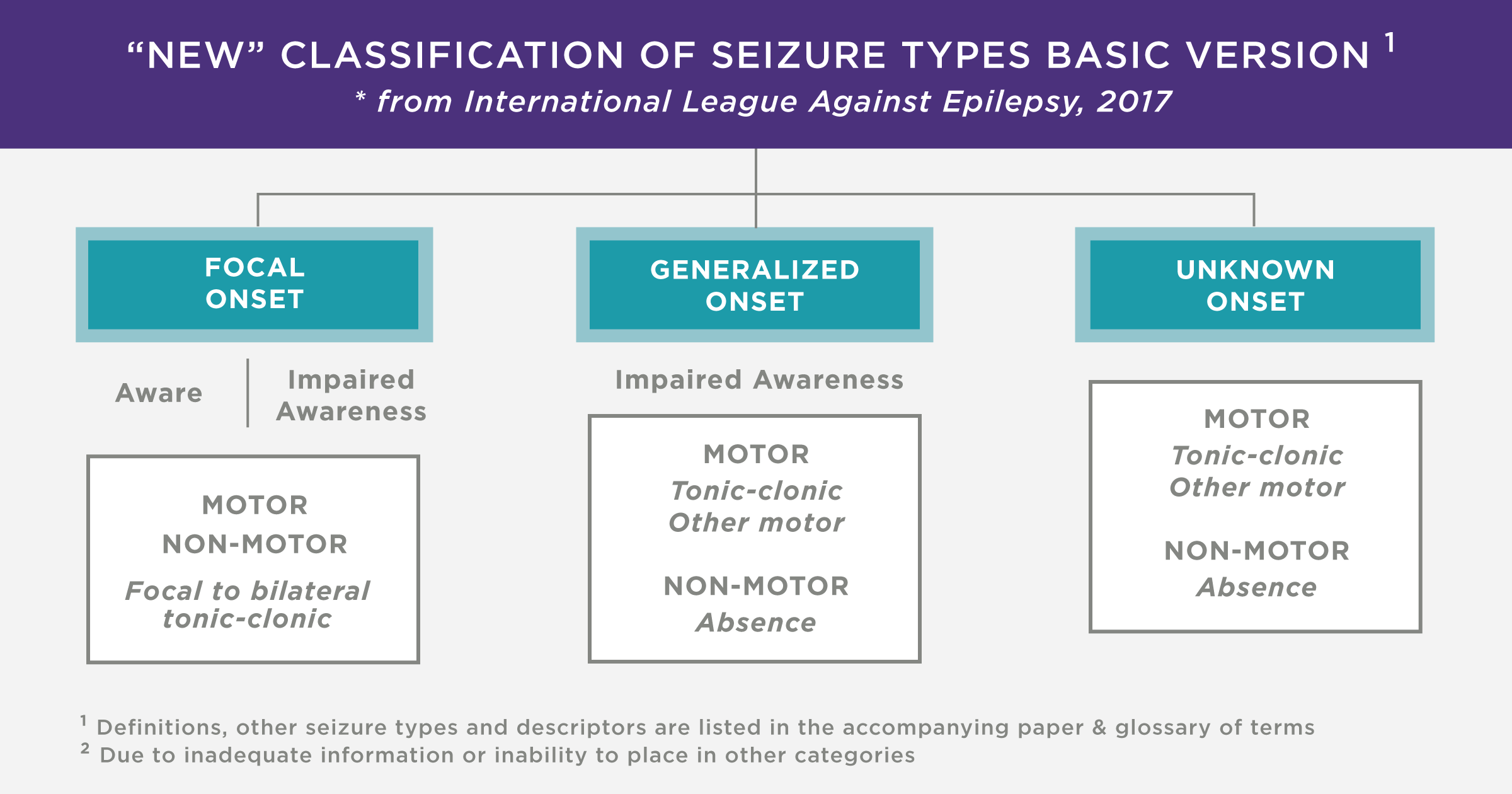
Epilepsy is a chronic non-communicable disease of the brain characterised by recurrent seizures generally brought on by specific triggers. The most widely accepted description of seizures is tonic-clonic seizures, in which there are brief periods of both tonic (stiffening) and clonic (twitching/jerking) muscle activity but epileptic seizures can manifest in a variety of ways, including absence or loss of consciousness.

My brother is one of the 50 million people worldwide who suffer from this illness and over the previous six years, he has suffered from sporadic, severe tonic-clonic seizures that have irreparably damaged his shoulder, necessitating a shoulder arthroplasty. I didn’t consider the long-term effects of epilepsy as a neurological condition on wider parts of the body until my brother experienced recurring seizures that damaged his shoulder. Upon further research, I have found that shoulder instability is a widely experienced deficit in epileptic patients due to the common risk of dislocation in a tonic-clonic state but can also be caused by the lack of education in seizure management, e.g. restraining someone’s arms during convulsions.
The most common type of instability seen in patients suffering from convulsive seizure conditions is a posterior dislocation alongside skeletal lesions, mainly reverse Hill-Sachs lesions. If the Hill-Sachs lesion covers more than 20% of the humerus head then a surgical procedure is the needed modality of treatment such as a remplissage procedure to fill the indent caused by the lesion or a bone graft to insert additional tissue into the humerus. However if it is not possible to reach clinically defined stability with other procedures or there is simply too much damage to the humerus, scapula and other bone tissues then a full or partial shoulder replacement will be considered. Reverse shoulder replacements are considered when considerable damage has occurred in the rotator cuff so that the replacement will rely on the deltoid to move the arm instead.


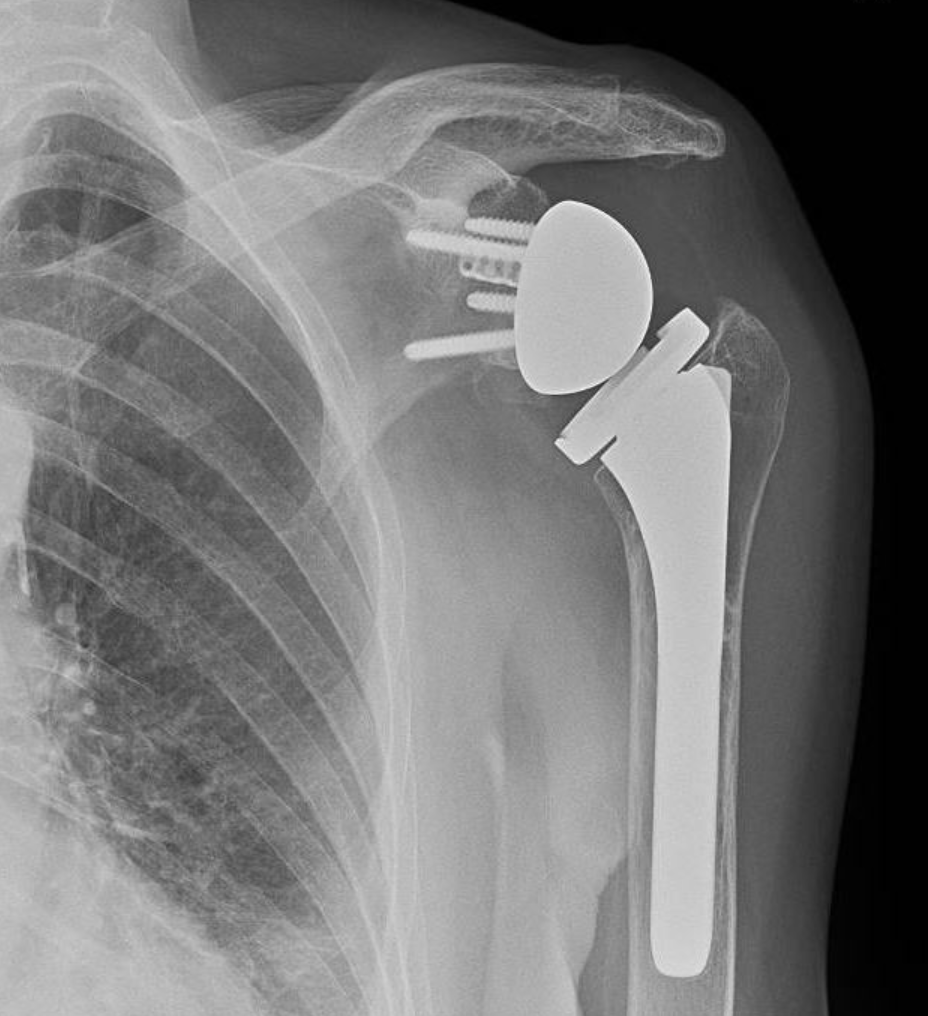
Some considerations to be addressed when importing an artificial shoulder into an epileptic patient range from seizure control during and post-operation, material compatibility, fracture and wear resistance and potential reoperation risks. In my opinion, the most important qualities needed from the shoulder replacement are high fracture and wear resistance due to the unpredictable nature of seizures making epileptic patients more prone to traumatic injuries. Furthermore, material compatibility is vital in ensuring the arthroplasty fully integrates with the patient and certifies a low risk of shifting during a convulsive seizure.
Material compatibility and fracture and wear-resistance are two factors that seem to work on a pivot as upon further research it seems that materials such as Ti-6Al-4V (titanium aluminium valium) alloys are less wear-resistant but are very effective in osteointegration and hold good osteoconduction properties. Up-and-coming research into joint replacements has already seen impressive benefits in using ceramic and pyrolytic carbons as alternative bearing materials and chemical modifications to polyethelene such as cross-linking, minimizing oxidation, and vitamin E impregnation, have been developed to minimize wear. Improving the bioactivity of orthopedic materials such as mechanically reinforced UHMWPE has been shown as successful and a great candidate to be used for bone replacements (Senra et Al, 2020).
To conclude, shoulder arthroplasty is a safe and beneficial surgical treatment for recurrent shoulder dislocation in seizure-prone epileptic patients (Austin et al, 2023). Upon asking my brother, he has seen a massive improvement in his quality of life thanks to the replacement surgery as he now has a better range of motion, reduced pain and increased stability without having to worry about complications if he dislocates his shoulder during a future seizure. I’d never considered the benefits of replacement body parts, such as shoulders, for patients suffering from neurological conditions but now I can see what is achievable in improving their quality of life when dealing with a debilitating disorder such as epilepsy.
Sources:
https://www.who.int/news-room/fact-sheets/detail/epilepsy
https://www.sciencedirect.com/science/article/pii/S1058274602000228?via%3Dihub#bib20
https://my.clevelandclinic.org/health/diseases/24304-hill-sachs-lesion#management-and-treatment

Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…