Following our lecture on sensors I was intrigued to find out more about the uses of Doppler Ultrasound in medicine. The body’s vasculature is complex and intricate, and serves a crucial role in keeping our organs and body alive. Ironically, this fundamental element for survival has potential to present a significant threat to life.
What is Doppler Ultrasound?
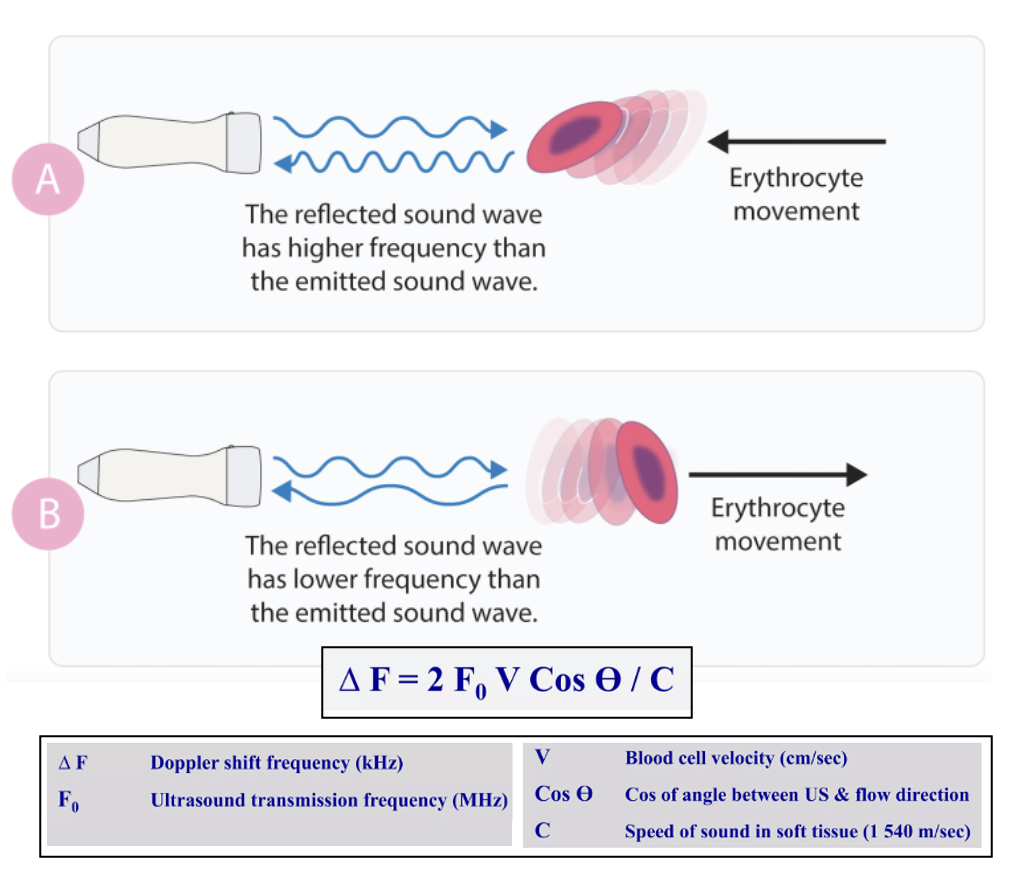
Doppler Ultrasound is a non-invasive method of measuring blood flow through a vessel using sound waves and is important in diagnosing conditions such as heart valve defects, aneurysms, and blocked or narrowing arteries. Additionally, Doppler Ultrasound is essential in monitoring blood flow in vessels before and after specific surgeries, including organ transplants, heart-valve replacements, and stent implantations.
A significant health concern?
After speaking with Marie, I became increasingly aware of how prevalent vascular disease is in the UK, with heart and circulatory diseases causing 26% of all deaths in England. That’s one death every four minutes! Vascular disease is severe and can result in poor wound healing, organ damage, stroke, heart attack, and even amputation of limbs. I had a discussion with Bethany, a student nurse who recently completed a placement on a Cardiac Intensive Care Unit. Bethany gave me valuable insight into the negative impacts that vascular disease has on both a patient’s quality of life and the NHS. I was shocked to find out that CVD-related healthcare costs amount to about £7.4 billion per year in England! This prompted me to question, “Could tissue-engineering replacement blood vessels serve as a viable option in the treatment of some vascular diseases?”.
Are they needed?
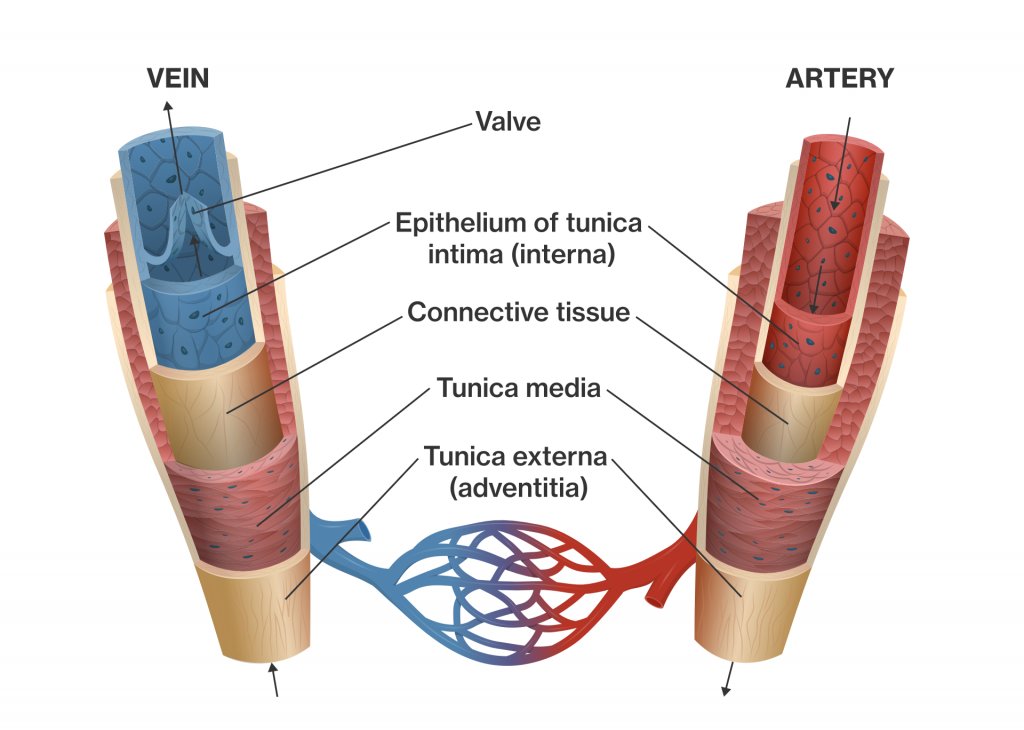
I looked into some current surgical treatment options and found that stents are commonly used to restore blood flow in a narrowed or blocked artery. However, when multiple arteries become blocked, an artery bypass graft may be performed using segments of healthy blood vessels from other parts of the body. “Would tissue-engineering new blood vessels be necessary if bypass grafts are usually successful?” I thought, especially when they would face a minimal risk of rejection coming from the patient themselves. After reflecting on this question, I concluded that tissue-engineered blood vessels would add value if successful. Some patients don’t have suitable blood vessels in other parts of the body to use in a bypass graft, and this shortage is a factor that could be overcome. Additionally, the vessel could be perfectly engineered to fit the patient and “grow” as they age.
How far away are we from successful tissue engineering of blood vessels?
Weinberg and Bell tissue-engineered the first blood vessel in 1986 using collagen, smooth muscle cells, endothelial cells, and fibroblasts. Adult stem cells are usually preferred as a cell source in tissue-engineered blood vessels over embryonic stem cells due to lower ethical concerns. I created a timeline with some key dates leading up to the development of the first tissue-engineered blood vessel to help organise my thoughts.
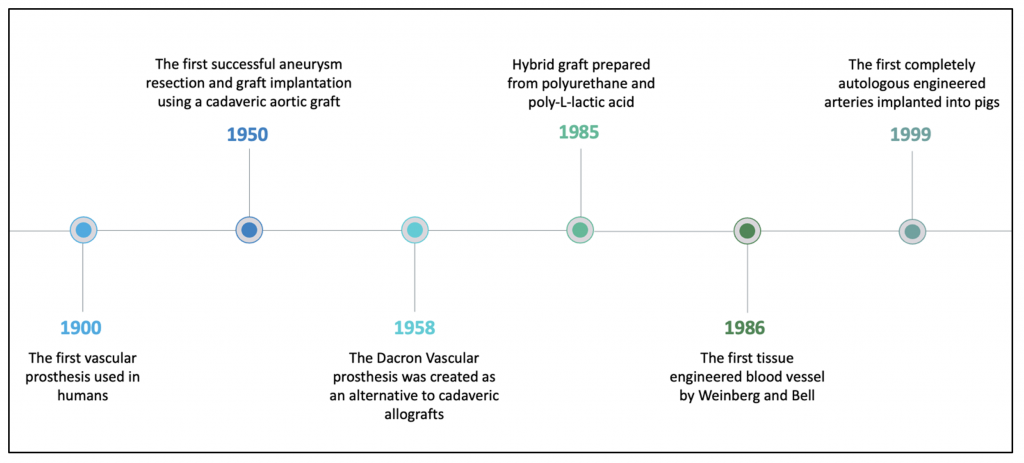
I was pleasantly surprised by the developments made through the years as blood vessels are such complex structures and this creates many challenges. Although progress has been made since 1986, there is still a long way to go before these blood vessels reach the clinic, but I believe we are not too far off witnessing significant advancements in vascular medicine.
Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…