Following a brief introduction in our lectures to sensors and prosthetics, I was inspired to learn more. Like many people, I had never considered all the limitations that affect prostheses users. I wanted to see how sensors could help make bionic limbs work as well as human limbs.
Controlling prostheses
In lectures we learnt about electromyogram (EMG) sensors which are used to control prostheses. To find out more I spoke to an engineering student who has produced a low budget EMG sensor as part of his year 3 project.
Improving Touch
When I think of a prosthesis, I think of a replacement body part. However, as the human body is deeply complex with many integrated systems to allow us to survive and interact with our environment, prostheses simply do not have the same functionality as human limbs. One thing I thought about was the extent to which upper limp amputees can experience human touch and their surroundings through their prosthesis.
Excitingly, by using a MiniTouch device, which can be integrated into existing prosthetic limbs, thermosensitive prostheses can be produced. Experimentally this device has been successful at allowing the user to decipher between objects with different temperatures. This technology helps prosthesis users to sense human touch akin to the feeling we get through our fingertips and increases sensation to help with motor control. However, the complete sensation of human touch still cannot be experienced by the user as human touch is a lot more complex than heat. For example, thermal sensors cannot convey to the user the texture of another person’s skin, although I was pleased to learn researchers are making progress in the development of tactile sensors.
The MiniTouch device technology has been developed further here at the University of Southampton. Researchers helped prosthetic wearers feel ‘wetness’ so both dexterity and motor control can be improved.
Improving Grip
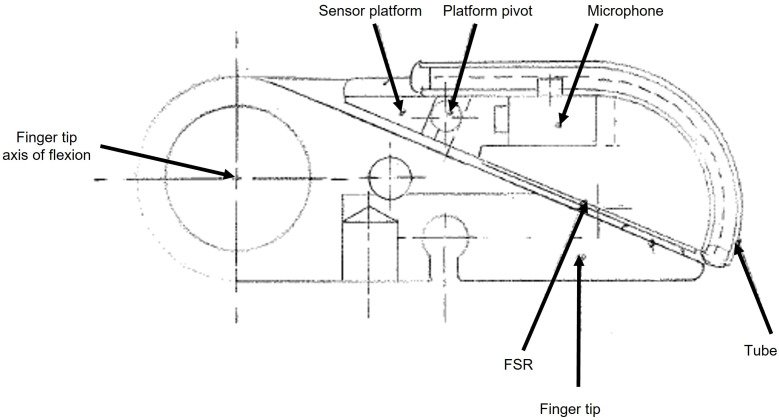
Sensors can also be utilised to improve the dexterity of prostheses users by preventing objects being dropped. This can be achieved by detecting when a slip is occurring. One option for slip detection is shown here. I found the reuse of existing technology and use of simple parts fascinating. It is made from a hearing aid microphone within a tube in contact with the grip surface. Slippage results in vibration signals which are transmitted to the air within the tube and onto the microphone. Airborne noises and interference signals can be thresholded out.
Controlling Orthoses
Orthoses are like prostheses but are designed to improve the functionality of movable parts of the body. There are many uses including rehabilitation and assisting daily activities. The mPower 1000, for example, is a neuro-robotic arm brace that fits like a sleeve on a person’s arm. It has sensors that can detect even a very faint muscle signal and the mPower 1000 provides motorised assistance in response. It is intended to increase arm movement affected by neuro-logical conditions such as stroke, spinal cord injury, multiple sclerosis, cerebral palsy, muscular dystrophy, and traumatic brain injury. Ethically, I worry if orthoses are widely used by able bodied people, it could have an untold impact on society and potentially even lead to weaponisation of the human body.
My Final Thoughts
It is really important to continue developing tactile sensors so protheses can become more like human limbs. Researching this topic has changed my perspective as I now understand we are a long way from having prosthetics which work as well as natural limbs however there is a great deal of ongoing research to improve prosthetics.

Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…