During our sensor lectors, the concept of an artificial pancreas was discussed. This stood out to me as my stepmother has diabetes and I had never really considered how having this actually affected her life. It also made me aware that I didn’t even know if she already used an artificial pancreas! Then through researching, I was drawn to the DIY artificial pancreas. I wanted to understand what this was and whether it was the most beneficial option in terms of cost, function and aesthetics.
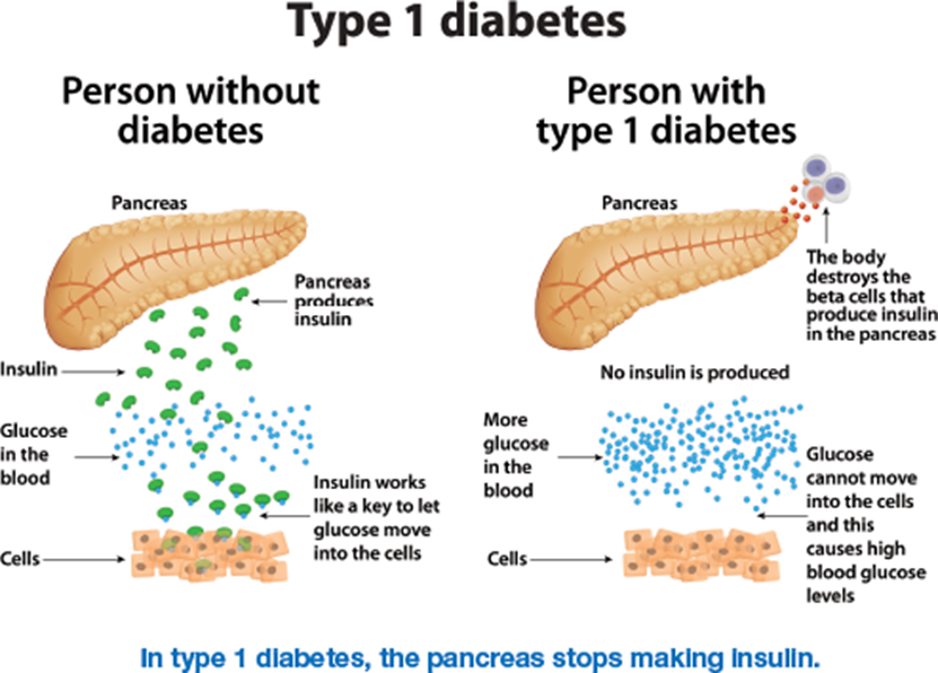
Individuals with Type 1 diabetes cannot produce insulin to monitor their blood glucose levels. Instead, they inject insulin throughout the day; calculating how much is needed dependent on factors such as what they’ve consumed.
What is an artificial pancreas and how does it work?
An artificial pancreas (also known as a closed loop system) can monitor blood glucose levels automatically, calculating and administering the required amount of basal (background) insulin. This is comprised of three components: a continuous glucose monitor (CGM) which uses tiny sensors under the skin that track the blood glucose levels every few minutes, delivering information wirelessly to an insulin infusion pump to administer insulin when the blood glucose levels is not within the target range as well as to a program on a device such as a phone to monitor the readings.
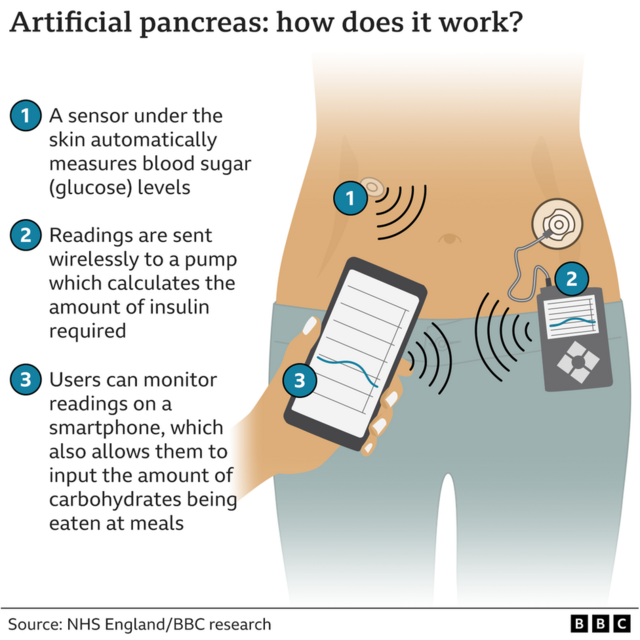
of the artificial pancreas and how they work.
https://www.bbc.co.uk/news/health-60133358
What is a DIY artificial pancreas and how does it differ?
A DIY artificial pancreas is non-NHS funded but uses similar equipment. It uses a specific app to control your equipment which needs to be compatible with your insulin pump. Guidance is mainly provided through the diabetes community and not the NHS as they have limited knowledge on how these programs work. If you are’ techie’ then you can fine tune this program and ‘train’ the system: making this an advancement on the NHS funded system.
What are the pros and cons?
Now, there are benefits to this: insulin is given automatically when needed which can be ideal especially for young children; allowing a more stress-free experience whilst giving their parents a way to monitor their blood glucose levels throughout the day. It also removes the need to inject which can be beneficial for those who dislike needles. As mentioned, the DIY version can be ‘trained’ to your specific needs so will reduce the energy and brainpower the individual spends on calculating the correct levels. However having said that, because it is technology, this can always malfunction and if given the wrong amount of insulin, it can cause a hypo. The program also requires internet connection where you still need to input your meals as the artificial pancreas can only give basal insulin automatically. In terms of the DIY version, it can be complicated to install and needs updating regularly. Since it needs to be attached to either a belt, a belt loop or a pouch, aesthetically the insulin pump can look bulky under clothing and limit the options of available outfits an individual could wear. This could cause insecurities or just be an added inconvenience.
After both points of views it’s clear how life changing a DIY artificial pancreas can be!
Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…