As my father prepares for his upcoming hip replacement surgery, I find myself reflecting on his fortunate access to private healthcare. The journey leading up to this decision has been far from straightforward. He has undergone numerous doctor’s appointments, consultations, treatments, and procedures, all aimed at providing relief from his debilitating condition. After exploring all other options, he has ultimately chosen to undergo the hip replacement surgery.
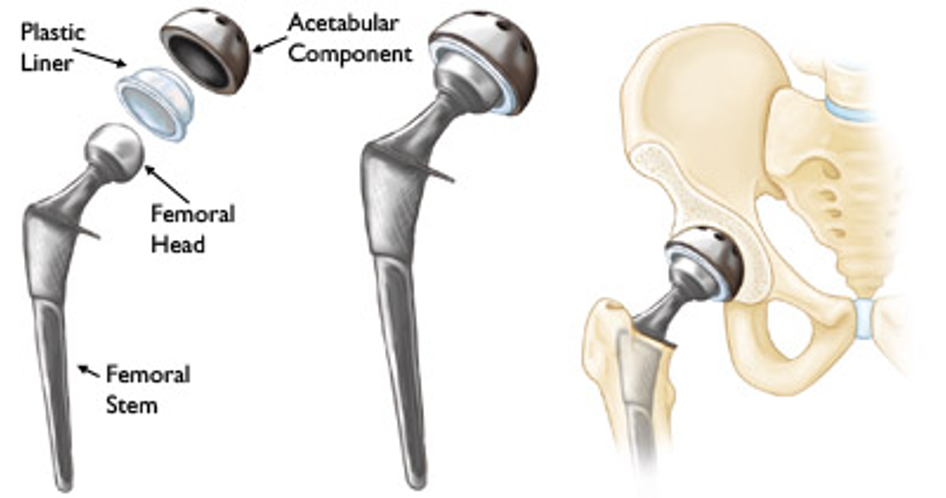
A hip replacement is a surgical procedure where a damaged or diseased hip joint is replaced with an artificial joint made of metal, ceramic, or plastic. By replacing the damaged joint with a prosthetic one, it not only relieves discomfort but also improves overall function, allowing patients to get back to their normal life, something that I am very excited for my dad to get back.
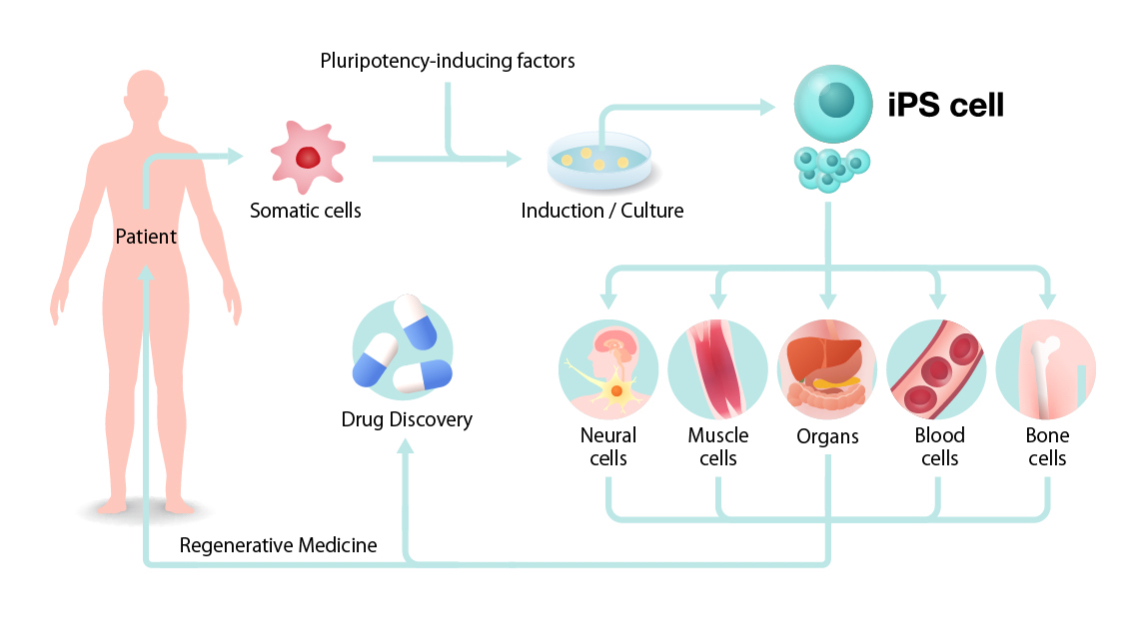
Thankfully, advancements in hip replacement technology have made way for significant improvements in recent years. Enhanced prosthetic materials, including durable ceramics and metals, now closely mimic the natural movement of the hip joint. New surgical techniques and tools such as robotics have all further contributed to these improvements. These innovations have revolutionised patient outcomes, offering swifter rehabilitation and improved quality of life.

Fortunately, my dad has access to private healthcare through his work and has therefore decided to proceed with the hip replacement privately. Although I am over the moon that my dad can get the care he needs quickly, it has got me thinking about the healthcare accessibility and disparities that exist within our healthcare system.
Not everyone has the luxury of access to private medical insurance. Patients undergoing NHS treatment for their hip replacement may endure lengthy waiting times for surgery. On the NHS website it states that the longest waiting time for a surgery should be around 18 weeks, but this is from the point of referral for the operation, and does not consider the time spent waiting to get the referral, which can be months! This can make the situation worse, diminish quality of life, and impose significant emotional and physical stress on patients and their families.
My dad’s hip replacement surgery is scheduled for next month. Reflecting on healthcare disparities leads me to question whether my dad would have been offered the option for such prompt surgery under different circumstances. I highly doubt it.
I decided to interview my dad to gather insight into his thoughts on his upcoming surgery and to understand the extent to which his hip affects his daily life. Additionally, I spoke with his colleague, Aubery Smith, who underwent a hip replacement surgery through the NHS to gain further perspective (transcript below).
While my father and Aubery Smith both have/ will have their procedures done at the same place, Aubery had to wait “approximately a year” to undergo his hip replacement surgery through the NHS. I cannot imagine enduring the pain he and my father described for such an extended period, and I strongly feel that changes should be made to address this disparity.
Overall, hip replacement surgeries have significantly advanced, offering individuals the opportunity to regain their daily lives pain-free, which is invaluable. However, I believe the healthcare system needs to implement additional measures, such as a reimbursement scheme. This would ensure that individuals in dire need of hip replacement surgery, whose quality of life is diminishing but lack access to private healthcare, can promptly receive the treatment they desperately need. Put yourself in their shoes; wouldn’t you look for timely treatment if faced with a similar situation?

:max_bytes(150000):strip_icc()/senior-woman-with-heart-attack-and-headache-fall-down-at-home-1183594716-b5da91d0fe9b45638d546820fafe8d13.jpg)











Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…