A metal implant is a biomaterial commonly used in orthopaedic surgery to help bones heal, or replace them entirely. Alloys are most typically used. They are designed to be non-corrosive, hard and durable – everything needed from the implant. In the photo below, the hip replacement one is probably the most recognisable, which 71,000 people in the UK have.

https://www.sciencedirect.com/science/article/abs/pii/S1286011518302479
Deciding on the make of the implant is very important. An article I read discussed how doctors need to consider what metals the patient has already been exposed to and what metals will be problematic, however a rejection can occur without any previous hypersensitivity. It suggests management strategies in the case the implant causes immune rejection. It states “Successful medical management with oral atropine sulphate has been reported in a patient with titanium pacemaker as well as with oral corticosteroids in a patient with titanium bioprosthesis for a spinal fracture”. This highlighted the importance of figuring out what metal to use in an implant, something I had not considered in much detail. The following link describes some types of implants: https://youtu.be/FfRZuNaKGdU?si=dT2X0tKhaC6ayGcF.
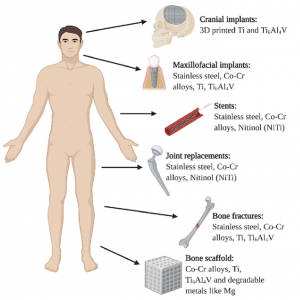
Image showing examples of types of implants
Patient’s reaction to the metal implantation varies dramatically. Some people show no rejection of the metal, others can show hypersensitivity to the metal and their body actually rejects it, causing intense pain and inflammation for the individual, potentially to the point that the implant has to be removed, but then what do they do to fix the issue?
Fixing the issue, but not completely…
Something which is used to reduce the risk of implants failing is covalently immobilising biomolecules onto the metal surface. An article in the Biomedical Engineering Advances journal believes that using a covalently attached immobilised biomolecule or not is a main determinant in the efficiency of the implant. Of course, this depends on what biomolecules are used and the patient’s individual differences, everyone’s immune system will react differently to the same thing. An example of an immobilised biomolecule is fibronectin, this forms an amide bond with the metal surface, others investigate Arg-Gly-Asp-containing peptides and ubiquitin.
A downside to the use of metal implants is stress shielding. This occurs when the bone density decreases as the stress load on the bone is reduced, due to the presence of the implant. This is a major issue for implants that will not be lifelong (a lot of implants – they do not last forever). This issue may not be apparent until after the metal implant is removed, such as after a severe femur break and the leg is significantly weaker and smaller.
So, what happens when metal implants do fail?
Well, in the UK, patients who’s implants fail, or cause harm, are able to bring legal action against the manufacturers and they are held accountable. The Nuffield Council on Bioethics in June of 2019 estimates ‘over 300 UK patients whose hip implants had failed brought legal action against the manufacturer under the Consumer Protection Act 1987’.
My opinion?
I believe there are lots of ethical considerations that need to be discussed at greater length. Since metal implants have lots of uncertainty surrounding their lifetimes and consequences (as most of it has not yet been seen) it makes it difficult for patients and doctors to make the correct decision, however this does not mean informed consent is dismissed.
You’ve provided good information on metal transplant use and drawbacks. However, while you included a paragraph at the end expressing your opinion, the rest of the blog lacks reflection. Consider why you’re interested in this topic, what prior knowledge you had, and how your understanding has evolved. Additionally, think about connecting it to your course. Ensure to use hyperlinks to cite your sources and create homemade visuals to enhance reader engagement.