Congenital disorders (more commonly known as congenital birth defects) contribute to a large portion of paediatric disabilities, and can persist into adult life, if the patient survives that long. The World Health Organisation (WHO) estimates that 240,000 newborns per year die around the world within 28 days of birth due to congenital birth defects. If the affected child survives beyond this stage, a further 170,000 children aged between 1 month and 5 years will die as a result of congenital abnormalities. So, why are these numbers so high? And what can be done to reduce them?
Video from the Centers for Disease Control and Prevention (CDC) explaining congenital birth defects.
As congenital disorders are usually identified after birth, when the abnormality has truly developed and “set in”, treatment aims to improve quality of life rather than cure the patient. Until now!
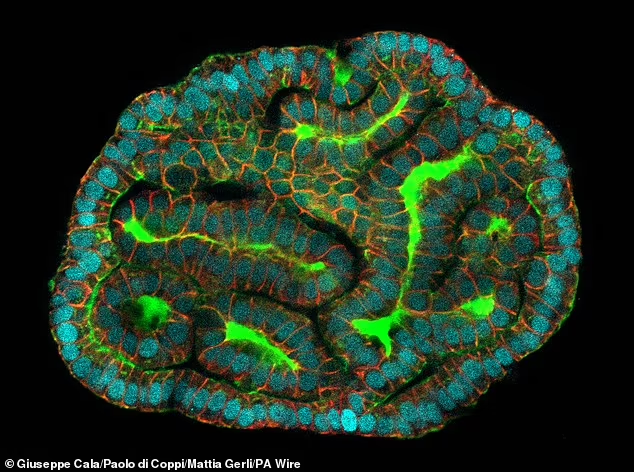
A “mini kidney” produced from stem cells in the amniotic fluid. Immunofluorescent staining reveals the presence of kidney-specific markers (e.g. GATA3 (distal tubule marker), LTL (proximal tubule marker) and ECAD (apical cilia marker)).
Scientific researchers from University College London (UCL) and Great Ormond Street Hospital (GOSH) have successfully extracted embryo-derived stem cells that are circulating in the amniotic fluid of late-stage pregnancies (i.e. up to 34 weeks), and developed miniature organs (so-called “organoids”) from these cells. Previously, foetal sampling in the UK has only been permitted up to 22 weeks after conception (which is the legal deadline for termination), hindering the ability to study late-stage foetal development. As the stem cells collected by the researchers are sourced from the amniotic fluid, rather than the foetus itself, it allows a ‘bypass’ of the legislation.
The research paper, published this week (March 4th 2024) in Nature Medicine, explains in detail the process of collecting stem cells from the amniotic fluid non-invasively, and culturing epithelial organoids that exhibit features reflecting their tissue of origin (i.e. small intestine, kidney and lung).
Video by Rajamanickam Antonimuthu explaining the process and potential of stem cell-derived ‘organoids’ in prenatal medicine.
This development is extremely exciting for prenatal medicine! The work provides a new opportunity to study late-stage foetal development (something which has not been possible before now), furthering knowledge and understanding. The organoids can also be used to model congenital disorders, extending knowledge on these, particularly in the later stages of development. Researchers now have the potential to develop new methods of diagnosis, prognosis and personalised therapy for congenital disorders, all because of a tiny little organ!
I find this research inspiring and highly interesting, as well as hugely promising for prenatal medicine. Anything that can help reduce the morbidity and mortality of congenital disorders is a huge step in the right direction. The researchers have since expressed their vision to extend the method into the production of organoids from mesenchymal and haematopoietic tissues, allowing the treatment of a wider variety of diseases. I am excited to see how this develops, and, who knows, maybe these tiny organs will be the key to curing congenital birth defects!
Your blog reflects your enthusiasm for the topic, which is great. You can enhance it by using WordPress tools like hyperlinks and homemade multimedia. Referring to multimedia can help explain concepts visually and strengthen your message. Try evaluating different pieces of evidence critically to support your arguments. Also, don’t forget to reflect on why you’re personally interested in the topic, how your knowledge has evolved, and the potential usefulness of future technology. Adding these elements will enrich your blog and make it more engaging for readers.