During a lecture and workshop focusing on prosthetics, I was intrigued by the design and functions of prosthetic limbs. Whilst watching the lecture, I spent some time wondering how the body communicates and works with the prosthetic to provide a function so similar to those of a natural limb in different everyday activities. Going into this research I didn’t have much prior knowledge and I perceived prosthetics to be limb replacements, but didn’t know their wider use. Upon seeing and interacting with a lower limb prosthetic in the workshop, I decided to further research this concept.
Types of prosthetics
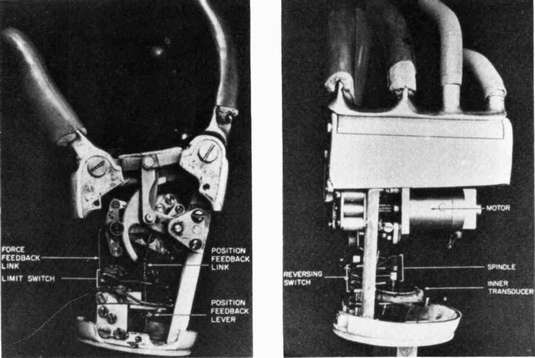
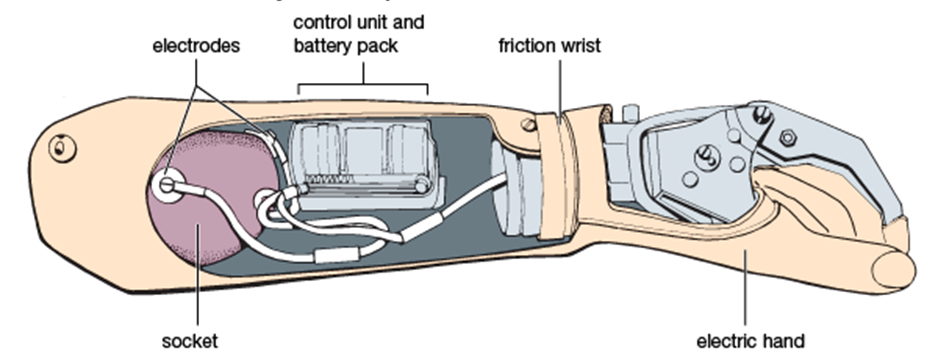
At the start of my search, I found there were many ways a prosthetic limb could work. Firstly, it can be powered by the body moving itself, e.g. where a cable may be placed on the shoulder and extend to a prosthetic hand. As the shoulder moves, the prosthetic moves. Secondly, it may have buttons, e.g. pressing a button on a prosthetic hand will cause the hand to grip an object. More recently, myoelectric powered prosthetics have been developed. This links muscles in pre-existing limbs to generate electrical signals and pulses via electrodes placed on the skin.

Prosthetics for different lifestyles
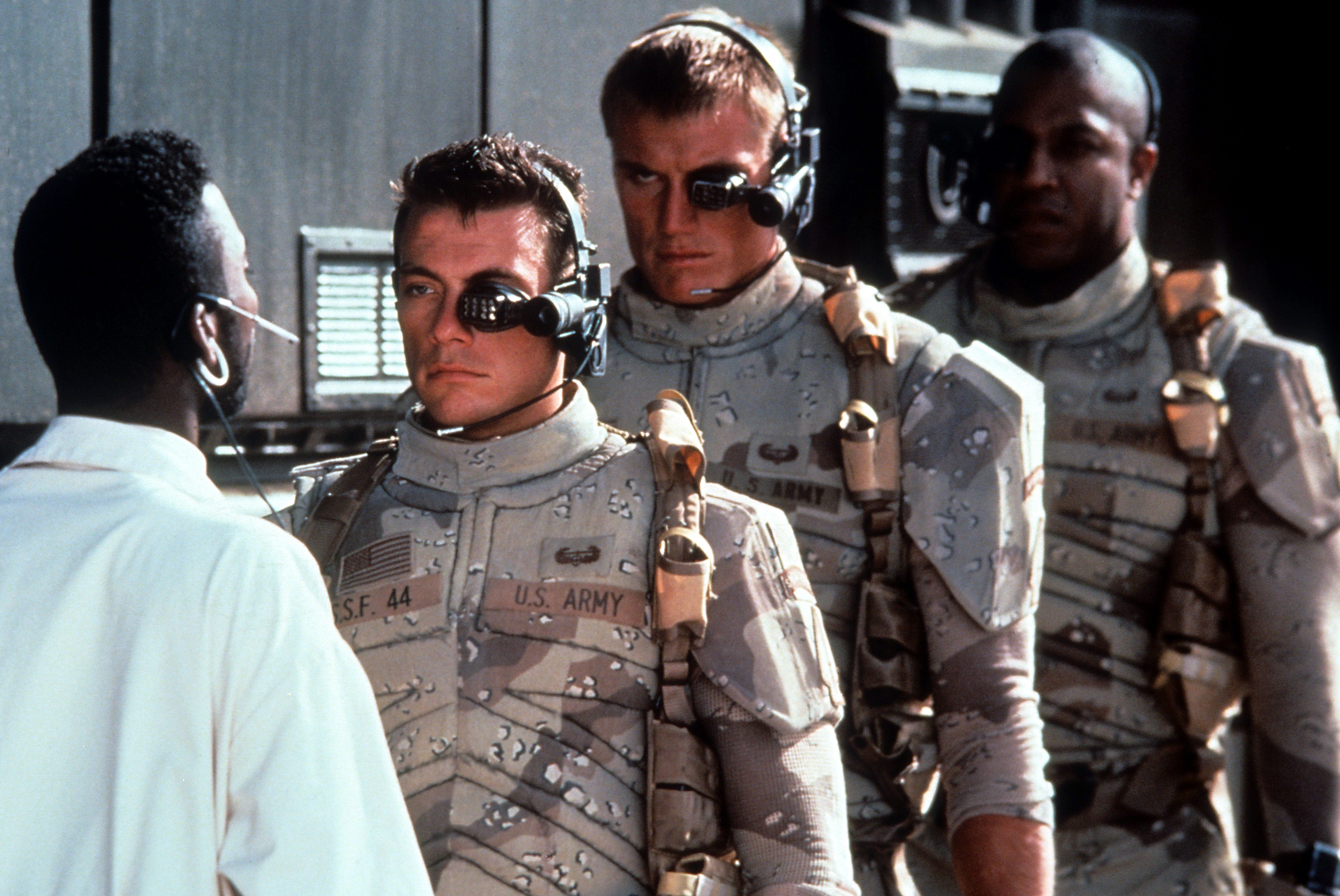
I then wondered how a prosthetic like these could be used in different scenarios and lifestyles, e.g with different hobbies. During my research I found the website Arm Dynamics which discusses the creation and execution of many prosthetic attachments for those with varied everyday lives.

Being an active gym goer I wondered how prosthetics could be used efficiently at the gym to complete exercises with correct form and came across Max Okun. Max is a personal trainer who was born without a left arm and forearm, but living with this through his life wasn’t going to stop him in his passions. It did however cause him injury as he was overusing his right arm, to counteract this pain, instead of surgery, he decided to use exercise to build up his muscles. It was therefore important for the engineers creating his prosthetics to ensure whilst Max was doing the exercises he was not causing further injury.
Max Okun Patient Profile from Arm Dynamics on Vimeo – This video shows Max using his prosthesis.
My reflections.
Researching this stream of engineering made me very grateful to be in a generation of such intelligent creators. As someone with fully functioning limbs, I think it is easy to take for granted how our brains are able to seamlessly communicate with our body parts. Even with tasks such as writing this blog, I require little to no thought in using my fingers. I can go bowling and tap dance without worrying about my mobility. I look forward to seeing what comes next in prosthetics and where it can go. Sitting this module has inspired me to look for careers that can aid in this development.





This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…