Context
Diabetes type 1 is a chronic and exasperating condition. Although I do not experience it myself, I have witnessed the tedious effect it has on lives. Management of diabetes is a growing field where further development of instruments such as the libre are becoming increasingly user friendly and accurate.

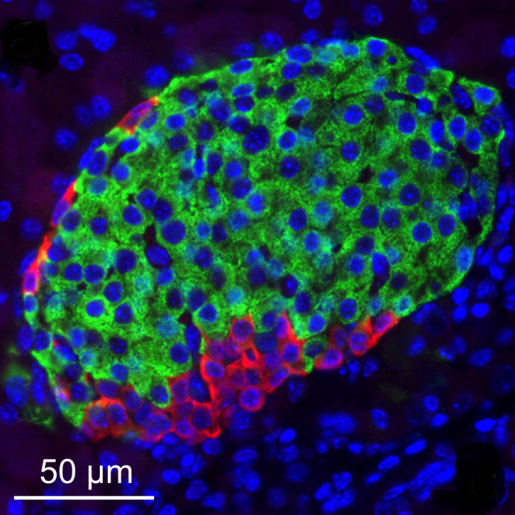
Witnessing someone close to me have to use the Libre and insulin pump daily, I saw how inconvenient the condition is; if there is a problem with the users ratios, their whole persona can change or their health turns to worse. I empathize with those who have to deal with diabetes day to day and those who may not find it as easy to manage because of other conditions. This module has nurtured my interest from lecture 2 as I have thought about the possibilities to either develop monitoring, or engineering of the beta cells themselves. The workshop station with Kirsten O’Brien and the tissue engineering lecture displayed to me how stem cells can be grown. These sprouted thoughts into allergenic cell transplantation and the complications of accessibility to pancreatic stem cells.
Current Research
There’s research into treating beta cells or replacing them using stem cells. Clinical islet transplantation has been explored – however there are issues with supply and demand, or quality of life for the patient, as they would have to use immuno-suppressants avoiding immune mediated graft loss/ potential organ failure. Materials such as scaffolding could be used in an islet transplant to protect from mechanical stress and aid the remodelling of the tissue.
However a controversy lies with, where do these replacement beta cells originate?
Complications Arise
Embryonic stem cells are the ideal candidate for use in this research, as there is higher replicability with differentiation and they have a success rate of up to 80%. The pleuropotency of ESC (embryonic stem cells) is the heaviest advantage as it allows the potential to replace faulty tissue. However, using these will result in the death of an embryo.
This raises ethical debates -when is an embryo considered conscious? Researchers can use aborted embryos with informed consent from the mother, although my mind goes to what happens to failed IVF attempts, hoping that the embryos would go towards research rather than discarded.
1.7 Million Human Embryos Created for IVF Thrown Away
Quote from the telegraph- This is outdated and not from a reliable source, however is still a considerable figure to give some thought about with bias.
Another complication to consider, is how to treat those who would refuse stem cell researched cures- because of religious views. In my opinion this should be heavily considered, as nobody should receive less medical care because of their faith, even if they refuse to accept the treatment. Would developing the Libre and pumps be an acceptable quality of life, or must induced pluripotent stem cells become further developed to avoiding these dilemmas?
From an economic standpoint, research into diabetes treatment would be a huge investment for the NHS. Evidence has shown that the NHS spends around £10 billion a year on diabetes. Shockingly, this equates to £25,000 a minute. Therefore not only would the quality of life be improved with research into a cure, but the government would also benefit, which I believe could be a huge motivator to diabetic research; quite sadist unfortunately. This makes me think further into whether diabetics would receive the research if they did not cost the NHS so much.
Summary Of My Thoughts
Reflecting on the impact this module has had on my thoughts about this, there are many options of research out there that could potentially cure type 1 diabetes, however the root of these treatments derive from a highly controversial source. From a holistic approach, using embryos would save many more lives than it would cost to research; however alternatives should receive more attention not just for ethical reasons but religious perspectives which can be overlooked in research and need more representation.
Further Information
https://www.science.org/doi/10.1126/science.abh1657– Scientific Article regarding topics discussed with higher scientific details.
Alternative Current Research
References
- Chung, H., Lu, Y., Oh, J., Wu, Z., & Im, K. (2021). Engineered bacterial outer membrane vesicles as a versatile platform for biosensing. Science, 373(6554), 148-153. https://doi.org/10.1126/science.abh1657
2. NHS England. (2022, March 16). NHS prevention programme cuts chances of type 2 diabetes for thousands. Retrieved from https://www.england.nhs.uk/2022/03/nhs-prevention-programme-cuts-chances-of-type-2-diabetes-for-thousands/#:~:text=Evidence%20has%20shown%20that%20the,effective%20in%20the%20long%2Dterm.
3. Priority You MD. (2021, May 7). What Is the Success Rate of Stem Cell Therapy? Retrieved from https://priorityyoumd.com/what-is-the-success-rate-of-stem-cell-therapy/#:~:text=The%20popularity%20of%20stem%20cell,biological%20component%20called%20stem%20cells
This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…