Limb regeneration is a field of research that captured my attention after Dr. Nicholas Evans’ lecture on tissue engineering. The thought of regrowing lost limbs or even organs, was once something only seen in science fiction (like Dr. Conners in The Amazing Spider Man) however thanks to the advancements in tissue engineering and regenerative medicine, it is now becoming a reality. The basic idea of limb regeneration is to stimulate the body’s own regenerative abilities to grow new tissue, bone, muscle, nerves and blood vessels. Many animals are already capable of this such as a salamander.

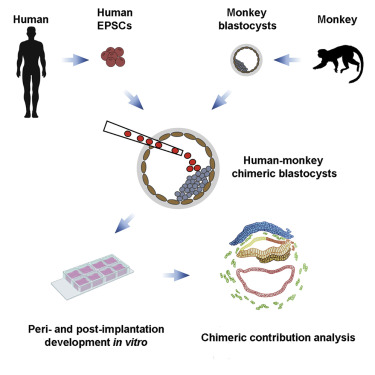
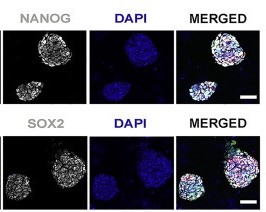
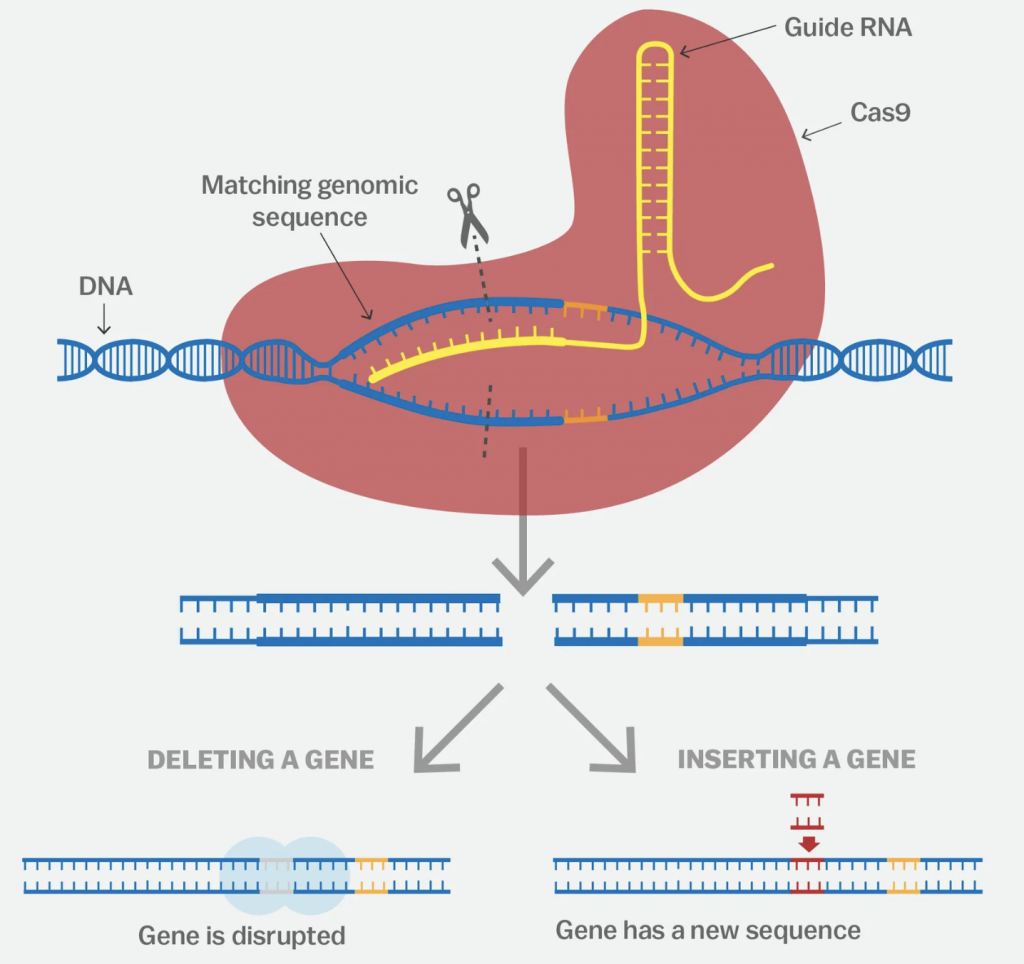
The process of limb regeneration starts with the formation of a blastema which is a mass of undifferentiated cells capable of enacting growth and regeneration into organs or body parts. The cells have been reprogrammed to become pluripotent. Once the blastema is formed, the cells differentiate into the various types of tissue that make up the limb. They are guided by a complex network of signalling molecules and gene expression patterns. The process is similar to the normal embryonic development of a limb but, it is much faster. While the possibility of regrowing limbs is exciting, it also raises some ethical concerns.
Developing new medical technologies and procedures is expensive and regrowing limbs is no exception! This raises the question of who would have access to this technology? Will it only be made available to the wealthy or to those with good insurance? This could further widen the gap between social classes so is this really necessary?
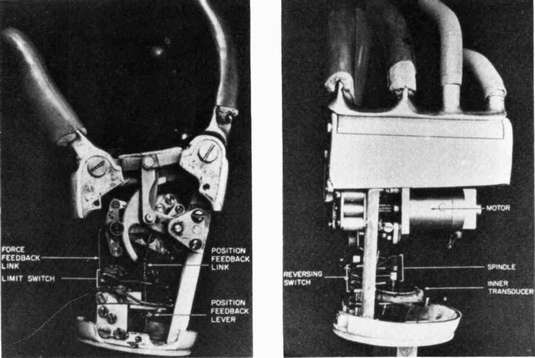
Another concern is the impact of limb regeneration on the existing prosthetics industry. Prosthetics have come a long way in recent years and many people have benefitted from the advancements in this field. However, if limb regeneration becomes a reality, what happens to the prosthetics industry? Will there still be a need for prosthetics or will they become obsolete? This raises questions about the economic impact of limb regeneration.
Perhaps the most significant ethical concern is the question of whether limb regeneration is even ethical in the first place. Some argue that it is playing God and that scientists and doctors should not be meddling with nature in this way. On the other hand, others argue that it is perfectly ethical as long as it is used for good and not for frivolous reasons like armed forces around the world creating super soldiers.
Despite these ethical concerns, there are many potential benefits to limb regeneration. For example, it could greatly improve the quality of life for amputees, allowing them to regain or gain lost functionality and independence. It could also decrease the use of prosthetics as I said earlier, which can sometimes be uncomfortable and difficult to use. Limb regeneration could also lead to advancements in other fields such as organ regeneration. I believe that the potential benefits exceed the ethical concerns as there are numerous applications of such a process and it would have a significant impact on human health and well-being.
In the end, the decision of whether or not to pursue limb regeneration is a complex one that requires careful consideration both the potential benefits and the ethical concerns. Limb regeneration is an exciting field of research that has the potential to revolutionise medicine and drastically improve the lives of many. With the points I have brought up and with your own opinion, I now ask you, should we use it?










This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…