Type 1 diabetes is a prevalent chronic illness with 1.4 million new cases in the USA per year. (ADA). It is a product of an insufficiency of insulin, caused by the autoimmune destruction of the insulin-secreting pancreatic β-cells. There is no current cure for Type 1 diabetes, however, there are a number of treatments to help cope with it.
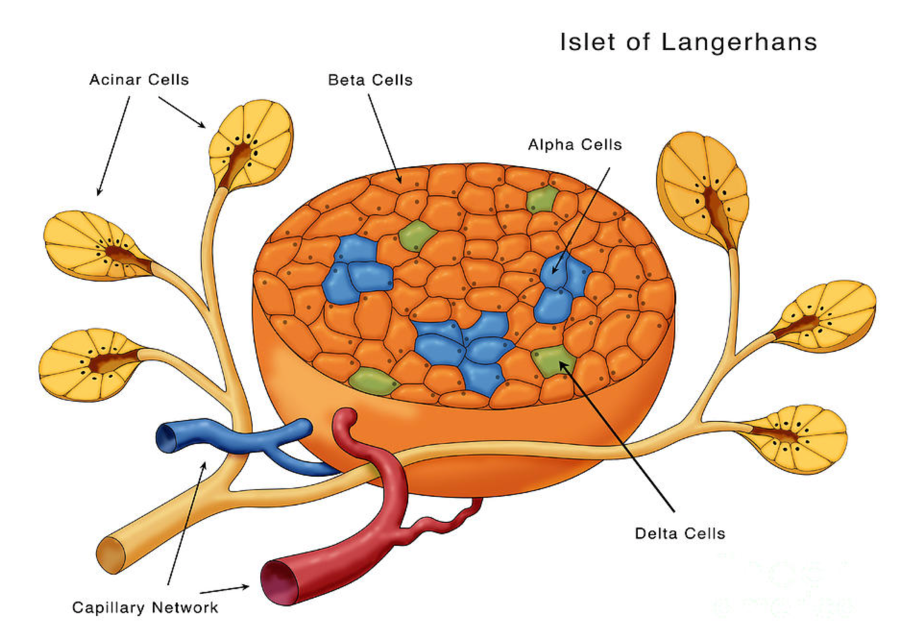
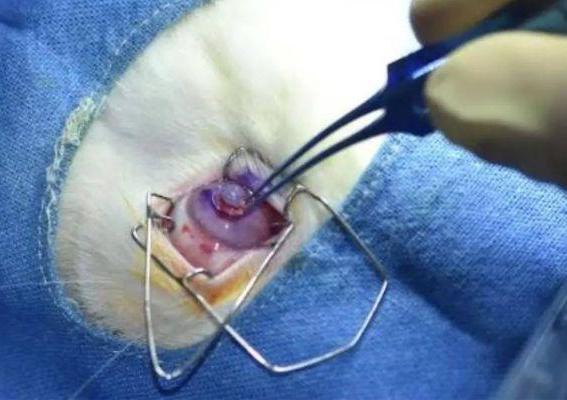
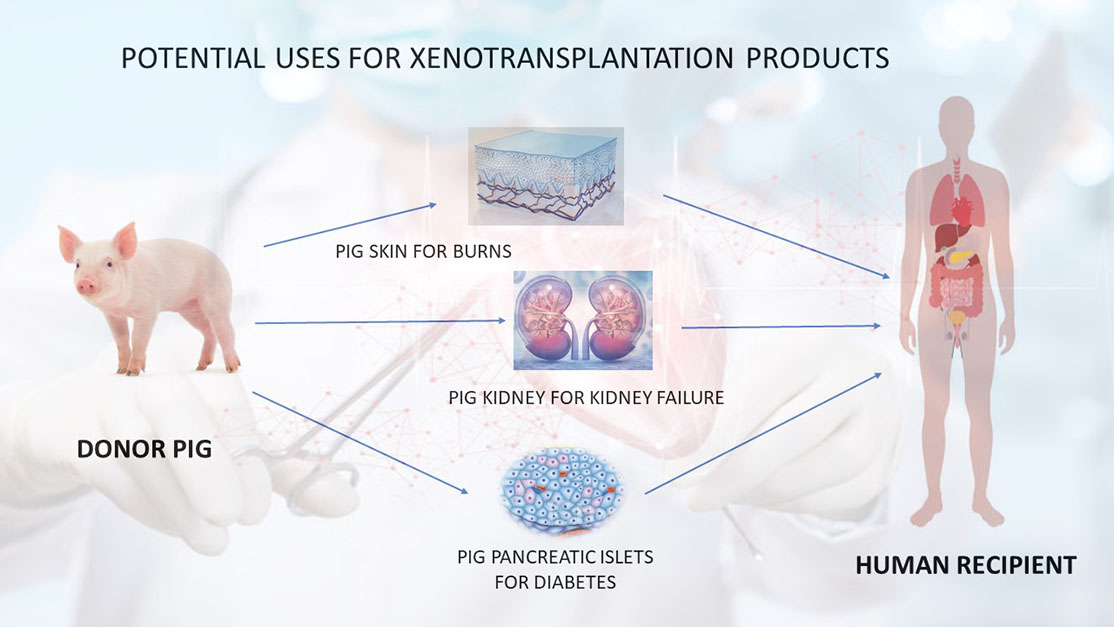
Islets of Langerhans are cells from human donors in the pancreas that secrete insulin and glucose and can continually control blood sugar levels when implanted in the liver. Islet transplantation for diabetes has shown to be less invasive and result in fewer complications in comparison to traditional transplantations.
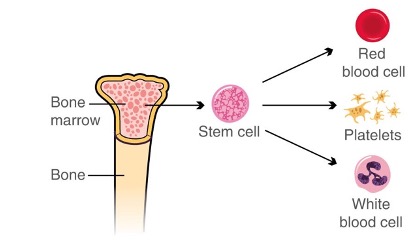
One potential cure for Type 1 diabetes is human embryonic stem cells (hES), which are cells that have the ability to efficiently and rapidly differentiate and are functionally similar to adult human islets. This suggests that hES cells may be a renewable supply of human β-cells that can aid to the development of cell therapy for diabetes (Kroon et al. 2008). A limitation in this domain is that there is a scarcity of donor tissue (Champeris Tsaniras and Jones, 2010), which can restrict the use of such therapies. This reflects the need for more donors to help treat those with this chronic illness.
In more recent literature, protocols have been created/improved to drive human pluripotent stem cell–derived pancreatic β cell growth (SC-β cells) through the stages of its development (definitive endoderm, primitive gut tube, pancreatic progenitors, endocrine, and β cells). Hogrebe et al. (2021) postulated the importance of the influence of microenvironment and cytoskeletal signalling on endocrine induction (both of which can influence the generation of these cells) that generate highly functional SC-β cells.
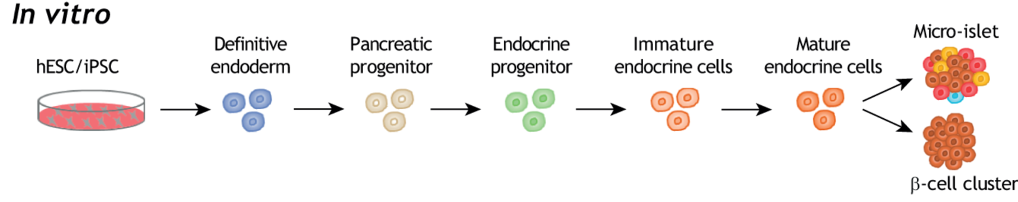
This not only simplifies differentiation methodology, but also improves outcomes for multiple cell lines. This is advantageous as cell lines have a longer life span, proliferate more quickly and are easily manipulated. These are important for complex tissues and allow for better examinations of alterations in structure, genetic makeup, and biology of the cell. Using this new information, Hogrebe et al. (2021) created the six-stage SC-β cell differentiation protocol for generating highly functional SC-β cells. This protocol recreates stages of embryonic development to achieve high SC-β cells maturity and differentiation efficiency. A limitation to note, however, is that this multi-stage process takes 5 weeks to complete, which can create possible problems that affect the successful generation of stage SC-β cells. Despite this, this paper has lay the groundwork for effectively generating stage SC-β cells from cell lines that didn’t work for other protocols. Overall, this has posed a positive impact on this research field and has pathed the way for improved protocols for cell generation and potential cures for Type 1 diabetes.

Final considerations:
Earlier in the module, my interest was captured when the lecturer mentioned stem cells and diabetes in week 2. With family attachments to diabetes, I felt an appeal to research further into this field. I never fully understood the burden diabetes can have on an individual, and I feel as if others don’t quite understand either. Therefore, reading more into this literature has only enriched my knowledge further and given me the opportunity to better understand the struggle.
One aspect that sparked my interest when doing my research is that there are developments for potential cures, which I didn’t realise there could be one. With advancing technology anything is clearly possible!
My take home message from doing this research is to encourage more people to donate donor tissue to help those with diabetes and that bioengineering technology and developments are only growing, which gives hope to those currently suffering with this chronic illness.
Reference list:
Champeris Tsaniras, S., & Jones, P. M. (2010). Generating pancreatic β-cells from embryonic stem cells by manipulating signaling pathways, Journal of Endocrinology, 206(1), 13-26. Retrieved Mar 6, 2023, from https://joe.bioscientifica.com/view/journals/joe/206/1/13.xml
Hogrebe, N.J., Maxwell, K.G., Augsornworawat, P. et al. Generation of insulin-producing pancreatic β cells from multiple human stem cell lines. Nat Protoc 16, 4109–4143 (2021). https://doi.org/10.1038/s41596-021-00560-y
https://diabetes.org/about-us/statistics/about-diabetes#sthash.F8fRkPqd.dpuf#:~:text=Prevalence%3A%20In%202015%2C%2030.3%20million%20Americans%2C%20or%209.4%25,American%20children%20and%20adults%20have%20type%201%20diabetes. accessed 6th March, 2023.
Kroon, E. et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat. Biotechnol. 26, 443–452 (2008).
Xin-Xin Yu, Cheng-Ran Xu; Understanding generation and regeneration of pancreatic β cells from a single-cell perspective. Development 1 April 2020; 147 (7): dev179051. doi: https://doi.org/10.1242/dev.179051
















:no_upscale()/cdn.vox-cdn.com/uploads/chorus_image/image/70056327/kidney_cropped.0.jpg)












This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…