When you hear the word eugenics, most people immediately think of the Nazis, but there are still a lot of modern-day ethical issues surrounding the ideas of eugenics. First, let us define eugenics:
‘the study of how to arrange reproduction within a human population to increase the occurrence of heritable characteristics regarded as desirable’.
Now using this definition, we can look at how it relates to what the Nazis did and while not the first-time ideas of eugenics were used, it is the most well-known. They used their ideas of eugenics to ‘euthanise’ those within the state who were deemed to be ‘incurably ill’. This included thousands of disabled people who were considered to be unproductive members of the state and after this followed the larger groups such as the Roma, Sinti, and Jews. Here eugenics were used to justify the death of millions as a way of ‘population control’ which is very clearly a hugely ethical issue. While most people are completely against the Nazi uses of ideas of eugenics, there are some who believe that eugenics could be utilised again today in order to help overpopulation.

I became interested in this topic after covering the historical elements in our ethics and law lecture, so decided to do some more research on the subject and how it affects the world today. During my research I came across the fact that in 2019, a group of 11,000 scientists signed a statement urging population control in order to slow down the death of the earth due to climate change. This idea that we should control the population in order to sustain resources is not new. However, these ideas have been trialled in the past with poor results, for example China’s one child policy that was implemented to stop the exponential population growth of the country actually led to more of an increase rather than slow its growth. While these ideas of eugenics follow on from historical ones there is a new form that we have seen develop in more recent years, the idea of designer babies.
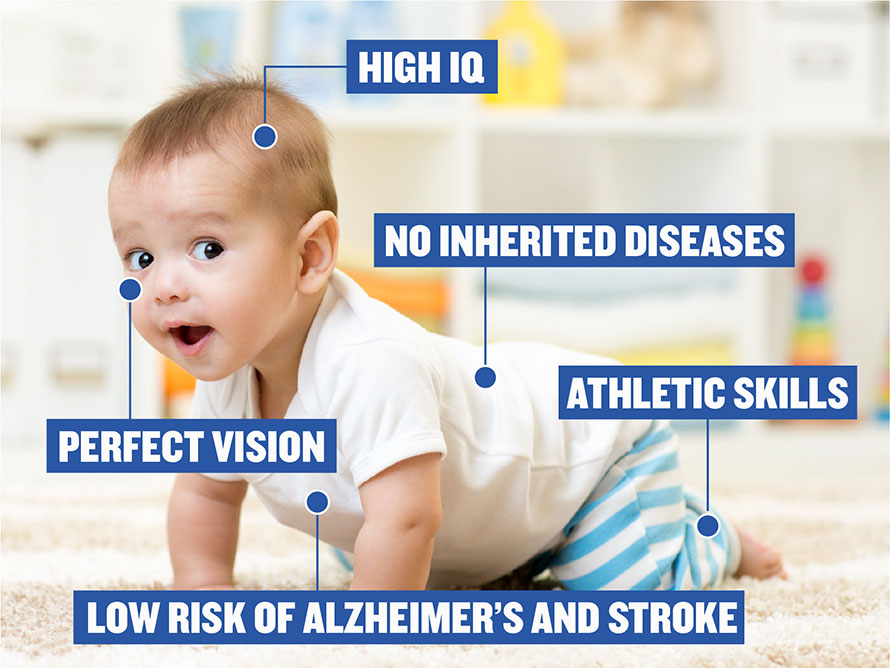
The concept of designer babies is where genetic testing is done on a child being created via IVF in order to determine whether they will have certain characteristics. The concept of designer babies is arguably the most ethically challenging as originally, this testing was done only to determine whether the child would be healthy, but it is now being used as a way for potential parents to determine whether the child will fit their expectations of that they want them to look like. I would argue that this is a new form of eugenics as it is allowing people to follow the idea of only creating children who have desired characteristics and as stated earlier, this is the definition of eugenics.
With these new forms of ideas of eugenics, it seems as though we have come full circle. From the Nazis using eugenics as their reasoning for murdering millions of innocent people, to modern day ideas of a way to protect our finite resources and then to creating IVF children with specific characteristics, eugenics seems to be an inescapable way of thinking. There is no way to justify these ideas as they put lives at risk. They fell under the radar as an ethical issue after WWII but with the concept of designer children and a need to protect our planet they are once again becoming an ethical issue within our society.











This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…