Upon starting my Engineering Replacement Body Parts module, the prosthetics joints and limbs lectures sparked a particular interest. It became evident to me that when an individual loses a fully functioning body part, alongside the obvious physical loss, there is also an element of mental loss in their sense of being. There becomes an immense divide between being ‘disabled’ and ‘able’.
Over half of the world’s population suffers from some form of cognitive, motor or sensory disease, and at what expense? The lack of efficient technology?
So… What if there was a way to enhance people’s capabilities beyond their losses, restore motor function and finally bridge that gap between limitation and potential? Luckily enough, we live in a period of time where there CAN be a way. A way we now call bionics.
Bionics is defined to be:
‘The science of creating artificial systems or devices that can work as parts of living organisms’
(Definition of bionics from the Cambridge Advanced Learner’s Dictionary & Thesaurus © Cambridge University Press)
By making it possible to replace whole organs to mimic that of the real ones, whether it be your eyes, ears, legs or even your brain, we are now able to massively improve the quality of life of those who have lost limbs, so they can freely go about day-to-day life like they once did before.
Bionic Integration with Hugh Herr
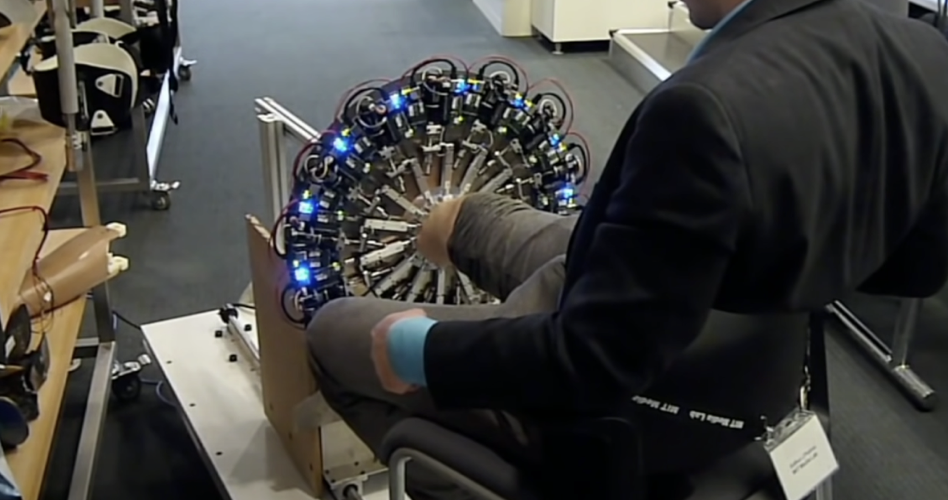
In an incredibly moving TedTalk in 2014, Hugh Herr explains how bionics shaped his life. After losing both of his legs in a climbing accident in 1982, technological innovation allowed Herr to cure his own disability with optimal support, and in doing so, discovered the beauty of the flexibility in the artificial part of his body.
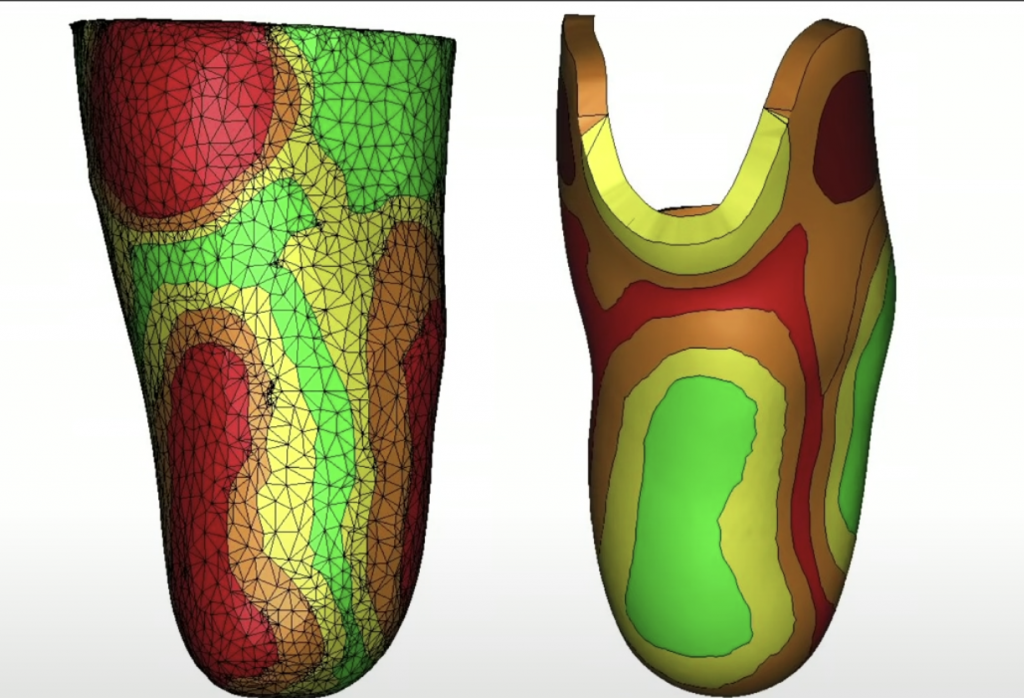
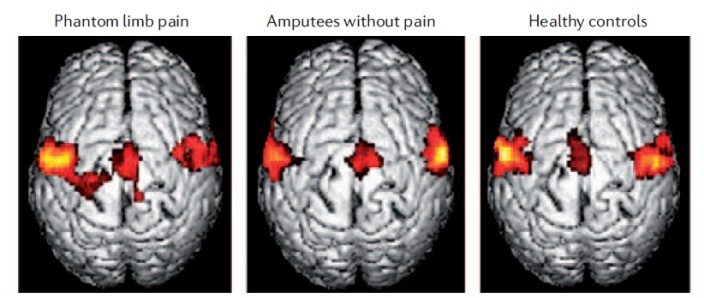
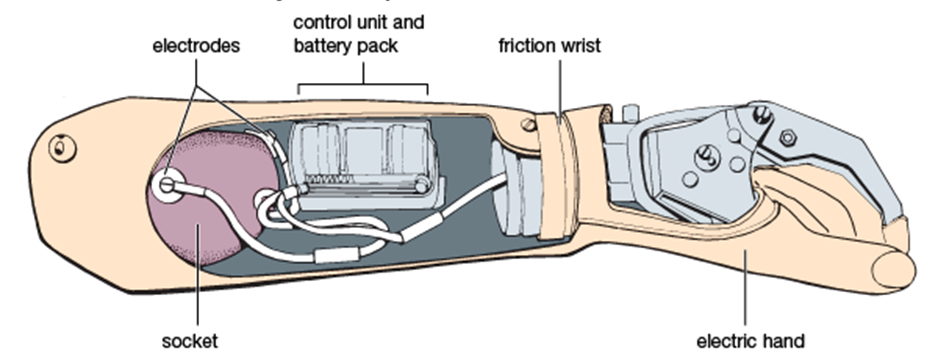
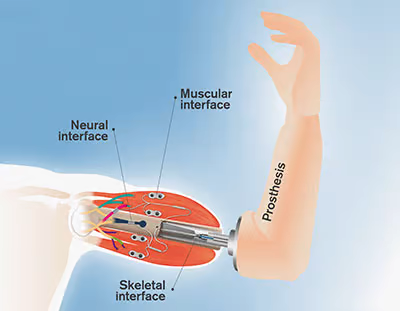
Through mathematical models, imagining and robotic tools, his bionic limbs were able to attach to his true body through synthetic skins with stiffness variations mirroring his underlying tissue biomechanics. To add to that, through bionic propulsion allowed the bionic limb to emulate normal muscle function, or even at an advanced level. This was critical for Herr and his athletic ability. To add even further, electrodes measuring electrical pulse of muscles communicated to bionic limb so if he thinks about moving, he moves!

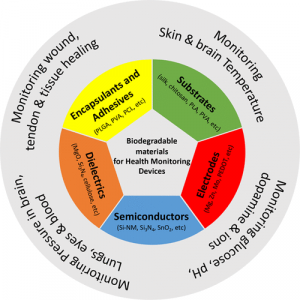
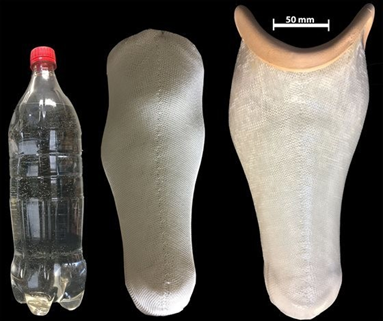
He took advantage of this flexibility and returned to climbing, eliminating his disability. Herr, as the head of the MIT Media Lab’s, is now building the next generation of bionic limbs and robot prosthetic that resemble biological materials.
The moral of the story is, despite losing both of his legs, the importance of bionics and the characteristic ability to use electromechanics attached to the body and implant them inside the body meant that Herr’s quality of life only flourished. He did not let it diminish him, nor destroy his self-wholeness. This should be the hope for all those who suffer from a similar story.
What do the ongoing advancements in ‘Bionics’ mean for the future of ‘disability’?
In decades to come, if the progress continues, we could see a world free of disability. Where a hand could have additional functional fingers, or an eye could improve low light vision and zoom in to make faraway objects clearer, or the paralysed can walk primarily based on artificial neural networks and swarm intelligence.
While artificial limbs are not nearly as good as a natural one, someday, we might advance to the point where artificial limbs might become superior to natural ones, available to everyone that needs it.

That being said, even those with normal physiology have appeared to use exoskeletal structures following the same principles to augment things like human walking, running, climbing etc. In doing so, it reduces metabolite cost and suggests that we are going into a time where these designs can make us stronger, faster and more efficient
To conclude…
Every being on this earth deserves a right to a life free of disability and full of ability at basic physiological function. The ongoing advancements of bionic technology show that as a human race, we are dependent on its growth to optimise our living. So perhaps humans cannot be disabled, but technology?








:focal(808x298:809x299)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/53/c3/53c3b6a3-929b-43f1-bf61-2d2cafbbecca/lacks1.jpeg)


This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…