So, when I picked this module way back in the summer of 2022, I had no idea that I would become engrossed in a world of engineering. I took biochemistry due to my complete lack of ability in physics, particularly mechanics. However, I soon realised this module ‘Engineering Replacement Body Parts’ dove into far more than the simplistic ignorant view inferred from the course name.
With the main areas of teaching being STEM cells, Prosthesis, Bionics, TISSENG and Ethics and Law I realised I would be receiving an answer to a question I did not know I had.
‘How does the potential of stem cells, engineered tissues and implanted devices in medicine impact the medical field as well as law and ethics in our society?’.
As a Biochemist the area that captured my interest the most was Ethics and Law and the rules and regulations around experimentation. Especially with the current rules changing on gender reassignment surgery for children which has sparked a lot of controversy on whether children can provide consent.
Within my course we have only briefly touched on ethical precautions when conducting experiments, which seems surprising judging how much they govern scientific research. One study that was only touched upon in a Neuroscience seminar I attended was the enforcement of electric shock therapy in the 1960s by Dr. Lauretta Bender. This was a known treatment for psychiatric disorders however she inflicted more than 100 children to shock therapy with the youngest being three years old! Maybe it was because my younger brother had just turned three or the fact that I couldn’t believe that it was not just adults subjected to this treatment. I suddenly thought about a child’s right to autonomy and further what makes someone fit or unfit to give consent.

It is easy to forget the significance of scientific regulations and ethical boards, as well as how some members of the scientific community only 50 years ago engaged in actions that would now be regarded as atrocities and unbelievable, as shows like Stranger Things and films like Suckerpunch almost trivialise and make medical scandals feel dystopian and alien to us.
The Government currently have legislation on getting informed consent for user research which is shown below directly from the government website:
If this had previously been in place many children would have been saved from the torment and emotional damage they ensued. There are three main views that can be taken when weighing up harm, benefit and autonomy.
- Libertarian
- Paternalistic
- Utilitarian
All of them would agree that low-risk research where participants are fully informed is an allowable argument. However, both a utilitarian and paternalistic argument would suggest that low risk research where participants do not know they are taking risks is justifiable. This is something I particularly struggled to understand.
Consent always seemed so black and white, simple yes and no, but when it comes to informed consent, how can a child be fully informed when they aren’t even fully formed?








This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
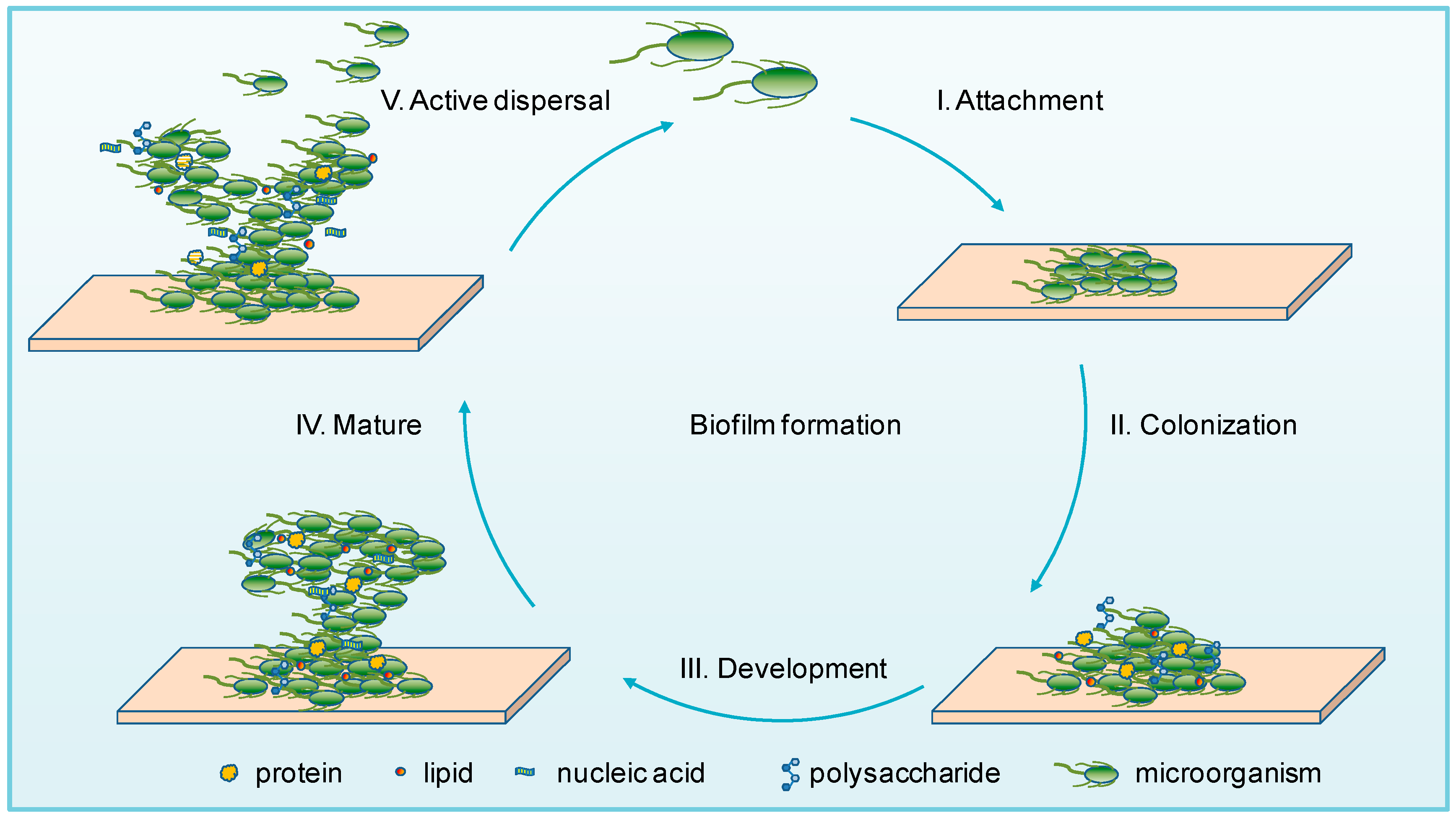
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…