I have always had an interest in the ethics behind scientific research, in particular the discussions around using human tissues in research. However, the case study of the Alder Hey Organs Scandal was mentioned in the law and ethics lecture and I had never heard of anything like it. It certainly piqued my interest as retaining children’s organs without consent or permission seemed such a baffling concept to me.
An ethical minefield

Alder Hey is an NHS hospital in Liverpool that was the centre of a scandal when in 1999 it came to light that during post-mortem investigations of children between 1988 and 19951, the pathologists were retaining the organs of the deceased children without the knowledge or consent of their parents2. This blatant “harvesting” of organs reminded me of a book I read recently entitled “Never Let Me Go” by Kazuo Ishiguro. To summarise, the book is the story of 3 children who grow up and realise they are clones of members of the public, and their role is to “donate” their organs until they eventually pass away. I found the dystopian science fiction nature of the book incredibly fascinating, and it shocked me how events that are eerily similar to those in the book have actually happened in most people’s lifetimes.
Why were the organs retained?
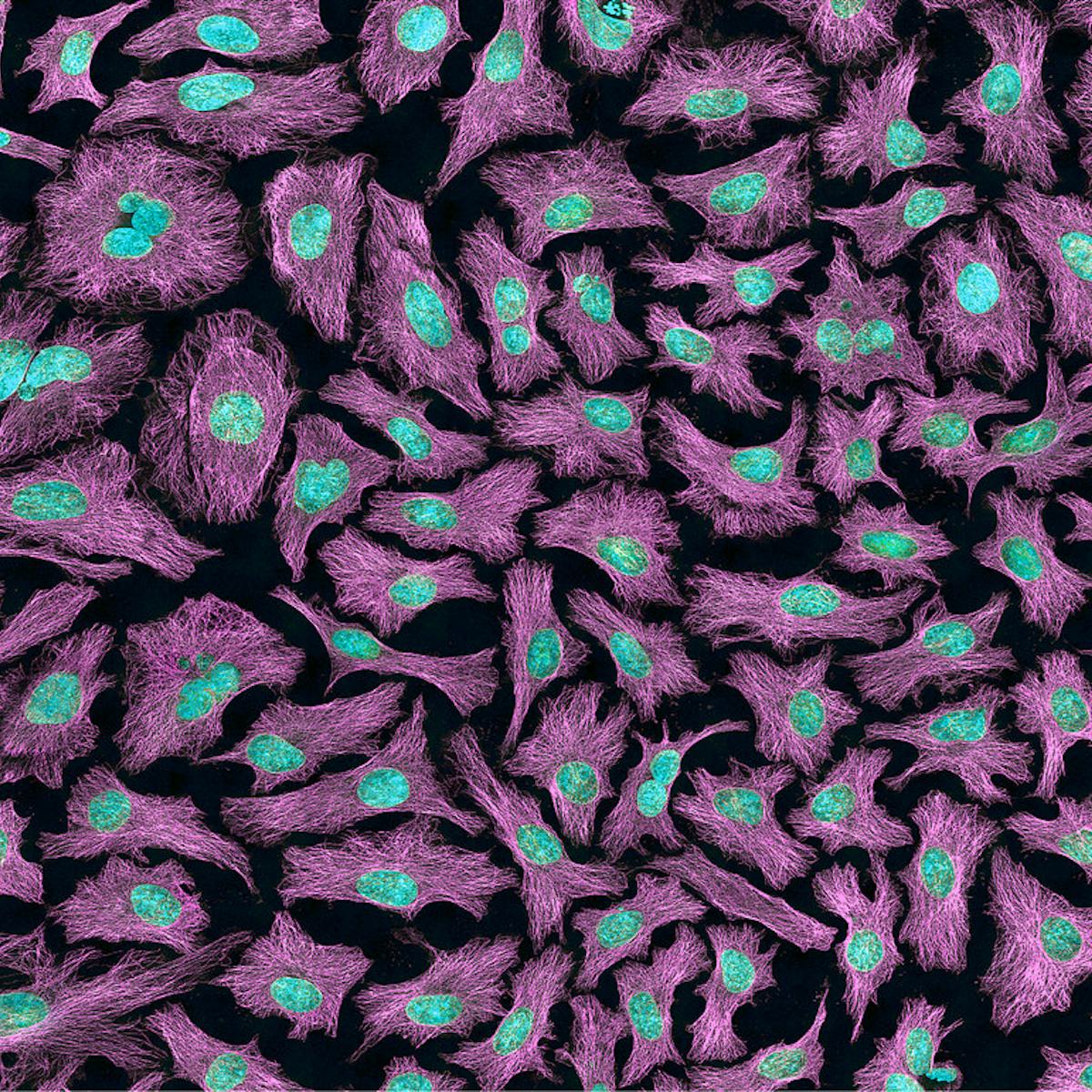
After the lecture I wanted to find out more about how activities that could well be described as “dystopian” managed to occur, bypassing the consciences of those involved. I initially assumed that the organs had been used for donations to children that needed transplants, but after thinking more about it whilst doing my research I realised that the organs would not be of use by the time the post-mortem occurred. Then why were the organs taken? Upon reading some journal articles from the years following the scandal I found out that many of the organs were not histologically examined, or used for educational and research purposes.

The reason the organs were retained (even for no apparent purpose) lies in the vague wording of the Human Tissue Act 1961 in which pathologists could retain tissues if there was a lack of objection, rather than informed consent. Therefore, by not informing the parents of the children about the reality of post-mortem procedures, there was a lack of objection and thus the ability to retain the tissues1. However, this cannot justify the utter devastation experienced by the parents of these children, who already had experienced the awful loss of a child, as they came to the realisation that their child had been incompletely buried.
Additionally, I researched more about Dr Van Velzen, who was mentioned in many of the papers I read. I discovered that he was a pathologist who was struck off the General Medical Council for storing over 1000 organs from 850 children in jars in a dirty cellar as they slowly decomposed3. This is a particularly uncomfortable revelation as it is practically impossible to justify the decisions made by Dr Van Velzen.
Moving forwards
I found researching this case further incredibly insightful because I was unaware of anything like this happening in the recent past, and there was so much to find out. Cases like the Alder Hey Scandal have a huge importance in future scientific ethics discussions to ensure history does not repeat itself. The scandal led to the Human Tissue Act 2004, which clearly outlines the need for explicit consent for retention of tissues for research or other reasons.

Reference List:
- Burton, J. L and Wells, M., (2002). The Alder Hey affair. In: Archives of Disease in Childhood (86/1). London: BMJ. pp. 4-7. DOI: https://doi.org/10.1136/adc.86.1.4
- Bauchner, H. and Vinci, R., (2001). What have we learnt form the Alder Hey affair? In: British Medical Journal (322/7282). London: BMJ. pp. 309-310. DOI: https://doi.org/10.1136%2Fbmj.322.7282.309
- Dyer, O., (2005). Alder Hey pathologist is struck off medical register. In: British Medical Journal (330/7506). London: BMJ. p. 1464. DOI: https://doi.org/10.1136%2Fbmj.330.7506.1464-a
:focal(808x298:809x299)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/53/c3/53c3b6a3-929b-43f1-bf61-2d2cafbbecca/lacks1.jpeg)
This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…