“Innovation is all about delivering real-life practicality that improves people’s lives” is a quote which I strongly believe, said by the founder of Taska, Mat Jury, and which I think exactly reflects the goal of each scientist in the biomedical field.

Damien Seguin, born and raised in France, is 43 years old and was the first disabled navigator to finish in the top 10 in the Vendée Globe. It is a non-stop and unassisted solo regatta around the world, thanks to which Damien has launched an important message: disability is not a limit, it resides only in the eyes of the beholder, but not in the heart of those who fight against it.
Damien was born with a pathology that prevented the physiological development of his left hand. He has always lived with his handicap, but he has been denied participation in sporting events several times until he was not able to found a team willing to support him in his greatest dream.The boats taking part in the Vendeè globe are IMOCA 60s, 60 feet long and extremely avant-garde. they are built specifically for solo racing and to be able to face the ocean without ever having to call for help from land. Despite his handicap, Damien hasn’t made any particular modifications to his boat “Group Apicil” except for having adapted the so-called “coffee grinder”, the winch column with which the sails are hoisted, retrieved and adjusted: he has a sleeve for hand prosthesis so that the left arm can also be used, but otherwise has the same equipment as the other skippers.

The sleeve was made of carbon, a high-performance material widely used in the nautical industry due to its extreme strength and lightness.
Thanks to Damien’s story, we can appreciate how, through advanced biomedical engineering, it is possible to tear apart the architectural barriers in sports and regain one’s own autonomy and strength. Sport is everyone’s right and that is why research and innovation must be supported and financed.
Prostheses in the sports field vary from the most rudimentary and least expensive like Damien’s to the most complex which can cost up to 60,000 pounds.
But what are the most recent advances in the field of sports prosthesis, and how much innovation has played a significant role in the performance of disabled athletes? In fact, each activity necessitates precise motions, a particular weight balance, and the usage of distinct muscles. As a result, unique prostheses for each activity have been researched in order to favor the athlete’s movements and enhance the comfort.
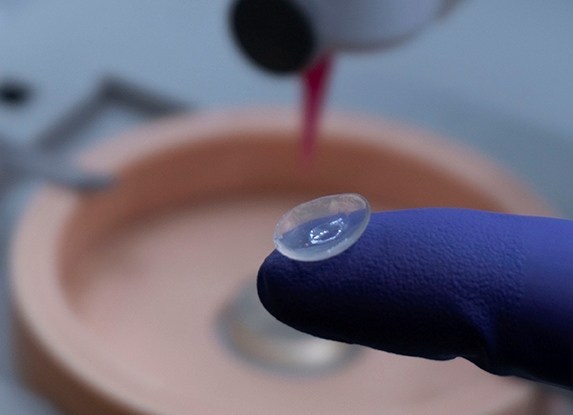
In the case of water sports such as sailing but also swimming, canoeing, fishing and many others, there is a need to have a support that is waterproof. TASK company is the first in the world to have developed a robust and waterproof hand. Highly technological, all fingers and the tip of the thumb are capacitive and can be used on any common touch screen. In the case of a sailor like Damien, it can be used to use all the on-board technological equipment mainly composed of screens for routing and weather.

This prosthesis can also be used outside sport, for all daily actions, but I believe that in the case of an athlete it can guarantee precision especially in gripping movements which must be quick and stable.
Certainly great strides have been made in the field of prostheses but in my opinion, in the future it will be necessary to achieve a level of comfort and accessibility such as to feel the prosthesis as an integral part of one’s body.
“the world’s first water-resistant prosthetic hand”









This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…