Total knee replacement surgery (TKRS) involves the removal of damaged and painful areas of the knee joint and replace it with specialised metal and plastic. A lecture by Dr. Nick Evans reflected on the disadvantages and problems with prostheses. He highlighted that internal prostheses comes with many issues, such a finite lifespan and can only be used for certain problems.
With this surgery comes many serious complications of joint replacement surgery, and these include: wound infection, blood clotting, malfunction of prosthesis or nerve injury. Upon reading these statistics, it made me feel inclined to research and find alternative, less invasive treatments for those in need of knee replacements.
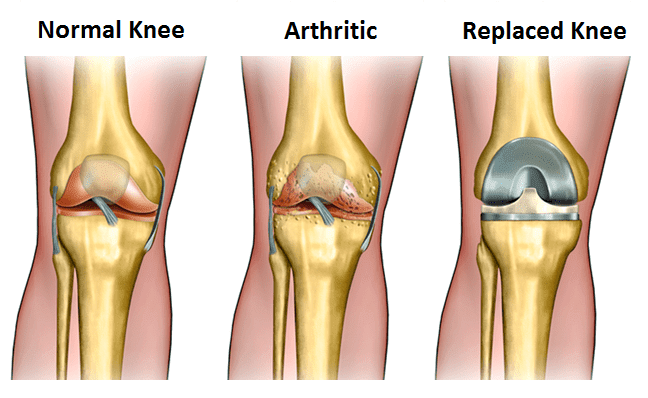
Knee osteoarthritis is a degenerative joint disease that breaks down joint cartilage and mostly affects middle-aged and older adults. It is the most common reason for knee replacement surgery, with 4.7 million estimated to have undergone TKRS in 2010. Mobility is significantly reduced and patients often experience constant pain even when resting. It is evident that this type of knee damage can be a burden for those suffering from it and I understand why people consider surgery to resolve it.
Common current treatment options
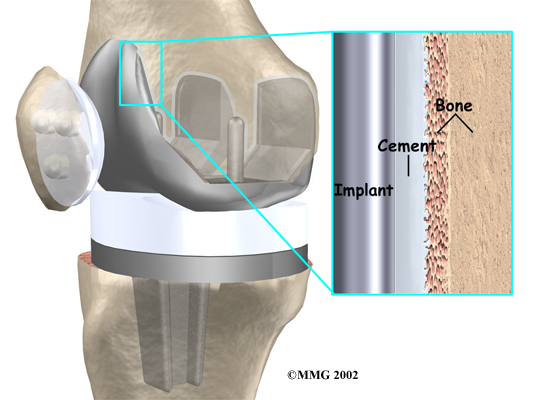
The most common surgical treatment for knee osteoarthritis is a cemented prosthesis. This is the process in which a layer of bone cement is placed in between the patient’s natural bone and prosthetic joint component. The advantages of cemented prostheses is that bone cement is fast-drying (10 minutes) upon application so there is confidence that the prosthetic is firmly in place, as well as early pain relief. However, with all surgery options, there are drawbacks. These include irritation of surrounding soft tissues and inflammation as a result of cement debris, and breakdown of cement can cause loose artificial joints in which patients would need to undergo another surgery. So if this current treatment for knee replacement is too invasive for the patient, then what other treatments are available that come with less serious complications and disadvantages?
Other treatment options
Something that shocked me was that there are many different alternative treatments for knee replacements. Here are some that particularly stood out to me, and ones that I would consider if I suffered from knee osteoarthritis.
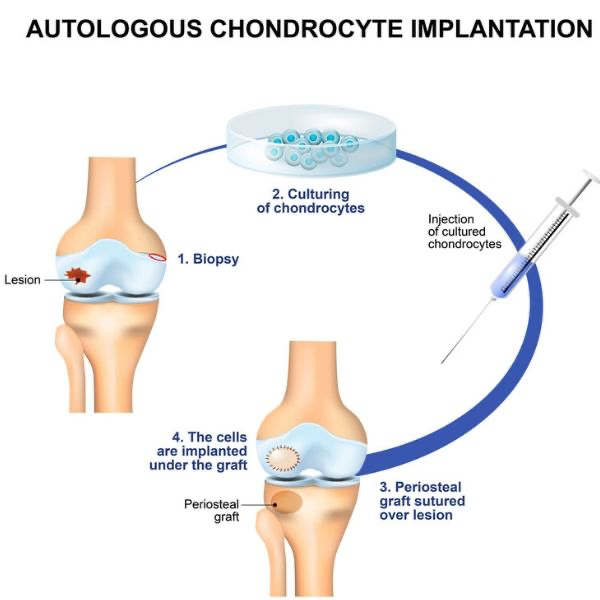
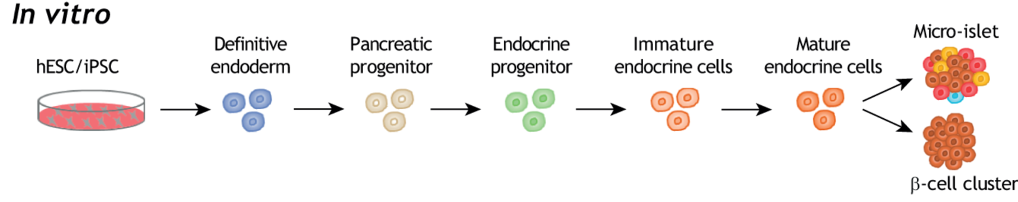
Cartilage regeneration is the replacement of cartilage instead of the entire joint for joints with limited arthritis. Autologous chondrocyte implantation (ACI) is a procedure that involves taking a sample of the patient’s cartilage cells, growing them in the lab and surgically replanting them into the knee. This may be a treatment offered for those effected by cartilage loss, with this implantation producing good/excellent results in 90% of patients with femoral condylecartilage loss (Minas and Chiu 2000). This may be promising for those who are looking at alternative treatment plans before fully committing to TKRS.
Current research has revolutionised TKRS with a new technique called the minimally invasive total knee replacement (MITKR). This involves smaller incisions than regular TKRS, which requires less muscle dissection and results in quicker and less painful recovery. This approach is said to have potential for dramatically reducing pain for muscles and tendons that have previously been cut during the standard TKRS. These benefits for this surgery has paved the way for less complications like less blood loss during surgery, and increased range of motion sooner after surgery. Overall, this promising and innovative minimally invasive total knee surgery has the potential to be the more commonly used treatment over others like cement prostheses. Video of this procedure can be found here.
Concluding thoughts
As I researched more into the field of alternate knee replacement treatments, I didn’t think that there were this many other forms available. I believe that it is beneficial for those in need of knee replacements to have many treatments available, especially for those that are unsure about fully committing to TKRS due to its invasive nature and serious complications. I personally would choose MITKR over the standard knee replacement surgery if I suffered from knee osteoarthritis, with its promising benefits and minimally invasive nature. With developing surgical treatments, such as MITKR, I will definitely keep up to date on the current and emerging treatments for knee replacements to further enrich my knowledge.

This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…