Recently I have been watching the tv show Alice in Borderland, which is set in an abandoned, seemingly post-apocalyptic Tokyo, where players have to complete dangerous to survive. One character, Akane Heiya, has a transtibial amputation due to an injury from a game and uses a running blade. I decided to look into how realistic her prosthetic is.
Obtaining the prosthesis
Since I was watching the show around the time I attended the lectures on prosthetics, it made me wonder where Akane was able to get a prosthesis, since I learnt from the lectures that the sockets are usually made custom for the shape of the residual limb. From further research, I also found that the residual limb often changes shape in the healing process and loses volume, and liners are worn between the limb and the socket to protect the skin which are changed daily (1). Akane wears bandages between her skin and the prosthetic, which could be changed regularly, but I don’t think it would have been feasible for her to find a fitting socket.

I did not think it would be realistic for her to find a running blade in an abandoned city. From looking into the availability of running blades I came across the Blade Library. This is a facility near the Toyosu Running Stadium in Tokyo which allows amputees to try running blades (2). There are 24 blades available to rent, as well as fitting workshops and and monthly runs to learn how to use blades (3). In the context of the show, it may have been possible for Akane to find a fitting blade here but would probably require prior knowledge of its location. However, I do think that the concept of a blade library is a really good resource to make running more accessible to amputees.
Using the prosthesis
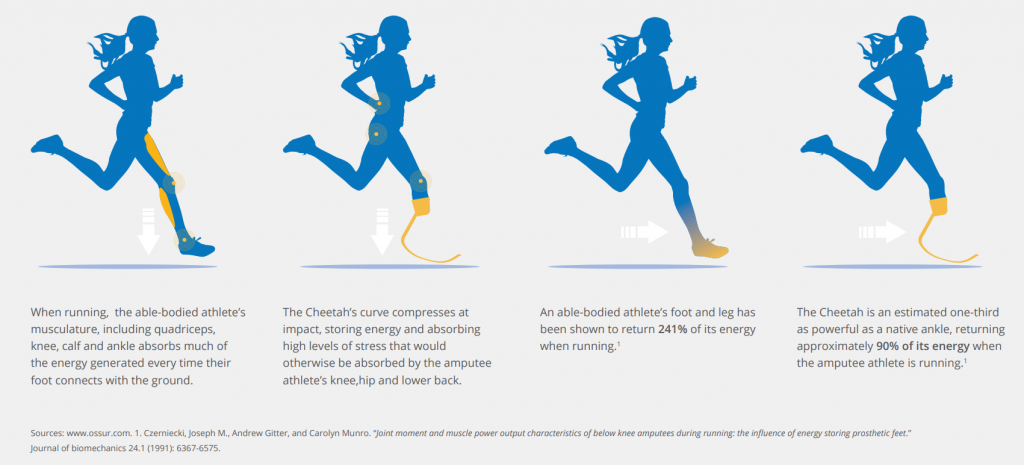
The prosthetic that Akane uses is a Flex-Foot Cheetah design (4). It is a carbon fibre running blade that is attached to the socket with a pylon connector (5). The curved blade stores the potential energy from the user stepping down into the blade and uses this energy to propel them forward (5). Akane uses a C-shaped blade, which is better for long-distance running than the J-shaped sprinting blades (6).
Although running blades are lightweight and durable, they are not made to be used as an everyday leg as Akane does. Running applies pressures to the residual limb in different areas than walking does, so wearing the wrong prosthetic for either activity can cause discomfort (7). They are usually slightly longer than the standard prosthetic to account for impact when running, and require slightly different alignment, so the knee has to remain bent whilst walking or standing (7).
Akane travel across different terrains and there does not seem to be a sole attached to her blade, so she probably would not have good traction on many of these surfaces. In the real world, Nike has developed interchangeable soles for running blades that can be clipped on and off for different terrains. These include rubber soles for the road and spikes for athletic tracks (8). These also help protect the blade to help them last longer.


Is Akane’s prosthetic realistic?
No, I don’t think that Alice in Borderland portrays a very realistic use of prosthetics, but I did enjoy looking more into prosthetic availability and finding out about the Blade Library. I think they could have included some scenes of her getting used to having a prosthetic and finding ways to get around some of the challenges to make it seem more authentic.
References
1. Infinite Technologies. Below Knee Leg Prosthetics. Infinite Technologies Orthotics and Prosthetics. [Online] [Cited: March 22, 2023.] https://www.infinitetech.org/below-knee-leg-prosthetics/.
2. Bailey, Joan. Athletic Prosthetics in Japan: Pioneers Pushing Boundaries. Japan Endless Discovery. [Online] [Cited: March 22, 2023.] https://www.japan.travel/en/tokyo2020/athletic-prosthetics-in-japan/.
3. Blade Library. Blade Library. Blade Library. [Online] [Cited: March 22, 2023.] https://bladelibrary.jp/en/.
4. Ossur. Flex-Foot Cheetah®. Ossur. [Online] [Cited: March 22, 2023.] https://www.ossur.com/en-gb/prosthetics/feet/flex-foot-cheetah.
5. National Paralympic Heritage Trust. Running Blades and their evolution. National Paralympic Heritage Trust. [Online] [Cited: March 22, 2023.] https://www.paralympicheritage.org.uk/running-blades-and-their-evolution#:~:text=Blades%20are%20prosthetic%20lower%20limbs,include%20%C3%96ssur%20and%20Ottobock..
6. Lacke, Susan. The Science and Controversy of Running Blade Prosthetics. triathlete. [Online] December 6, 2020. [Cited: March 22, 2023.] https://www.triathlete.com/culture/the-science-and-controversy-of-running-blade-prosthetics/#.
7. Gane, Jamie. Running – Blade XT vs Standard Prosthetic Foot. Jamie Gane Adaptive Athlete. [Online] February 14, 2018. [Cited: March 22, 2023.] http://www.jamiegane.com/blog/2018/2/14/running-blade-xt-vs-standard-prosthetic-foot.
8. Fox, Brinkley. Road Ready: Nike Sole 2.0 x Össur Running Blade. Nike. [Online] October 18, 2021. [Cited: March 22, 2023.] https://www.nike.com/gb/a/proof-of-concept-nike-sole-ossur-running-blade.



This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…