Recently I have had the privilege to come to Prof. Douglas Dunlops’ clinic, where I have gained a lot of understanding on orthopaedic surgery. One thing that interested me the most was looking at the development and evolution of hip replacement strategies, and where it can lead us in the future, hence why I have decided to write this blog.
From the beginning
Sir John Charnley was the first to research and develop total hip replacements. He aimed to create a total hip replacement using a synthetic substance between the femur head and the socket, instead of using the natural synovial fluid. After failed attempts with PTFE, Charnley eventually used Ultra-high-molecular-weight polyethylene (UHMWPE) for the first time in 1962. After five years of observing his patients Charnley announced the method as safe, allowing other surgeons to use his patented design and officially making the first functionally total hip replacement. After Charnley’s patent lapsed over 100 kinds of hips were licences, one of them being the EXETER. Its success arose from its tapered stem, allowing it to be easily popped out and replaced, but even-though 92% of them last over 30 years, hip prosthetics still seem to fail.
Less history, more science

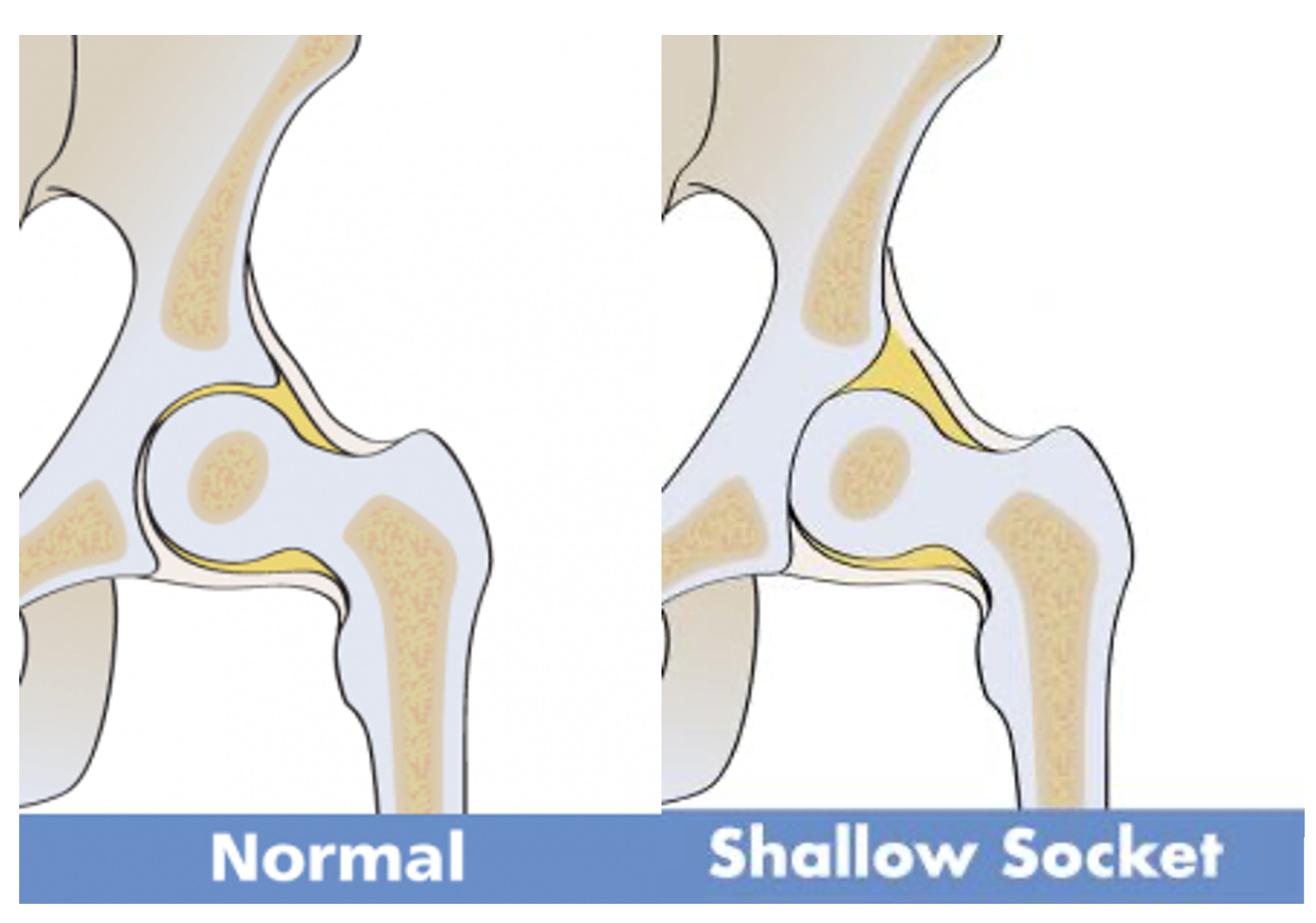
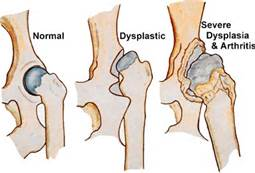
Prof. Douglas Dunlop gave me a lot of insight on all the reasons why hip replacements fail, but one that stood out to be the most and seemed to reoccur was corrosion. The same way the natural femoral head of the hip joint erodes with time, the synthetic joint can cause wear and tear of the cartilage, leading to the formation of a shallow socket and osteolysis. On top of that, physical shearing forces slowly remove the protective film on the metal surface, and any taper interference will corrode the metal further.
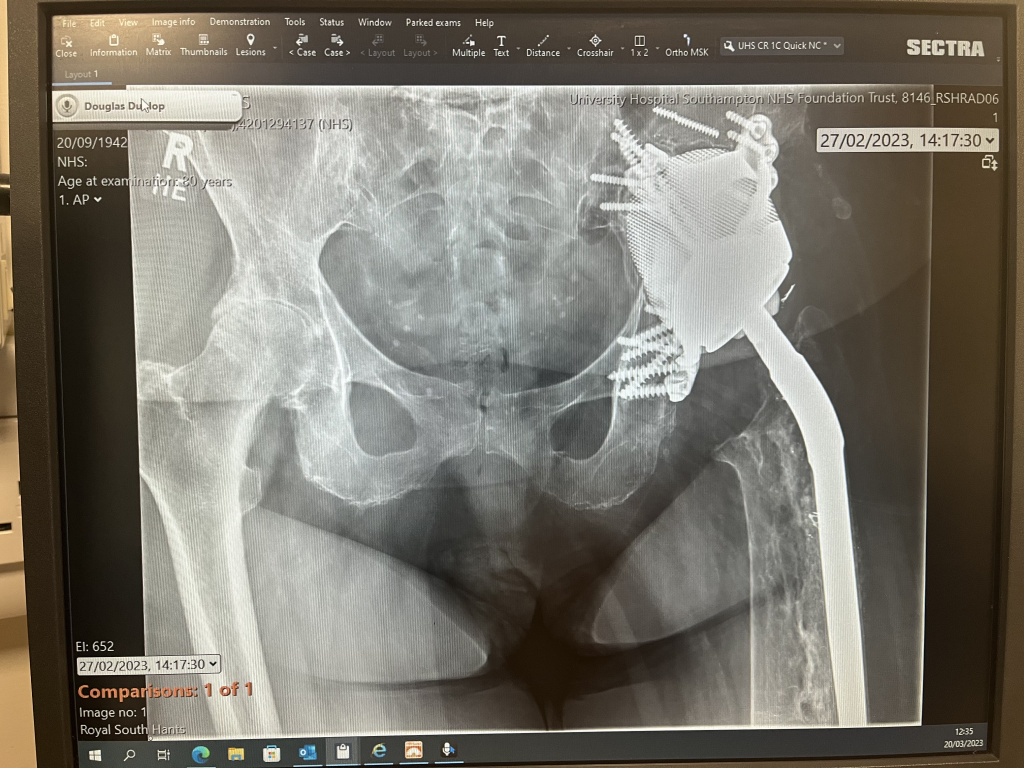
Prof. Dunlop also showed me an x-ray of an elderly patient who had undergone multiple hip replacement surgeries. The shallow socket of the patient caused by hip displasia required for the the prosthetic to be ‘screwed’ into place along with cement loosening. Each time the stem was replaced, the femur had to be reamed, increasing the risk of fracture, prosthetic loosening and infection. This patient had a 3M Capital hip, which prompted the national joint registry due to its poor performance. At the time, the Southampton General hospital was also using a CPT Zimmer brand prosthetic with a fracture rate of 3.4%, giving them a low rating on the registry. In order to overcome this issue, Prof. Dunlop, alongside researchers at Southampton University came up with a solution.
The future of prosthetics
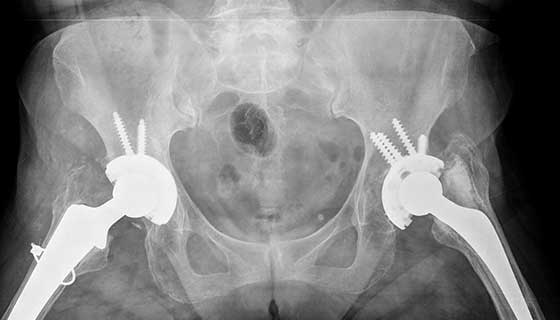
35 years ago, another patient at Southampton General had a similar issue. Her prosthetic migrated and became loose, leaving behind a gap in the bone. In 2003, bone graft from the bone bank was used, but eventually that also failed as screws loosened and the femoral head migrated. It was clear to me that any other attempt at revision would also be unsuccessful, but Prof. Dunlop told me about a new cutting edge technology that has the potential to change prosthesis for ever.
To overcome this issue, 3D custom implants were used, and held in place using stem cells. Not only is the shape of the implant a precise shape for the patient, but the stem cells act as a ‘glue’, allowing for bone formation and encouraging regeneration of the surface layer of damaged cartilage. The removal of old prosthetics may leave behind scar tissue, therefore stem cells may be the only solution to a patient where biology has failed. Upon further reading I have discovered that Dr. Daniel Wiznia of Yale University has developed a similar approach, and deduced that stem cells are a credible strategy and have considerable potential in the future of prosthesis.
Moving away from monoblock stems and exchanging them for a stem with an exchangeable ceramic head seemed to me like a very impactful advancement, but after hearing about the use of 3D printing and stem cells, it has become clear to me that scientists are not done there. It is fascinating to see how the approaches to prosthesis have changed in the last 60 years, and leaves us to think where it can lead us in the future. By writing this blog I aim to show just how fast science is progressing and how successfully scientists are coming up with solutions to clinical problems.
This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…