The stem cell and regenerative medicine workshop introduced me to a new advanced tissue engineering discipline: the use of microbubbles. I was fascinated to learn that many disorders are incurable due to drug delivery transport implications and that the development of microbubbles has the potential to solve many of these difficulties.
Microbubbles (MB) are non-toxic and biocompatible technological structures that interact dynamically with organs at the cellular level. They have a size of 0.1- 10 µm and can be destroyed by ultrasonic radiation (US). The US can be targeted to specific locations, improving selective therapy. Tissue engineering with biomaterials is an innovative and promising technique for increasing human life expectancy, and scientists are interested in integrating MBs with scaffold architecture.
Alzheimer’s disease (AD) is the most common cause of dementia. It affects around 50 million individuals globally, and its prevalence is expected to double by 2050. There are currently no treatments to cure Alzheimer’s disease, although the FDA has approved drugs to treat symptoms. E.B White, the author of my favourite childhood novel Charlotte’s Web, is a notable person who sadly died of Alzheimer’s disease. He has suffered by losing his freedom and forgetting his accomplishments.
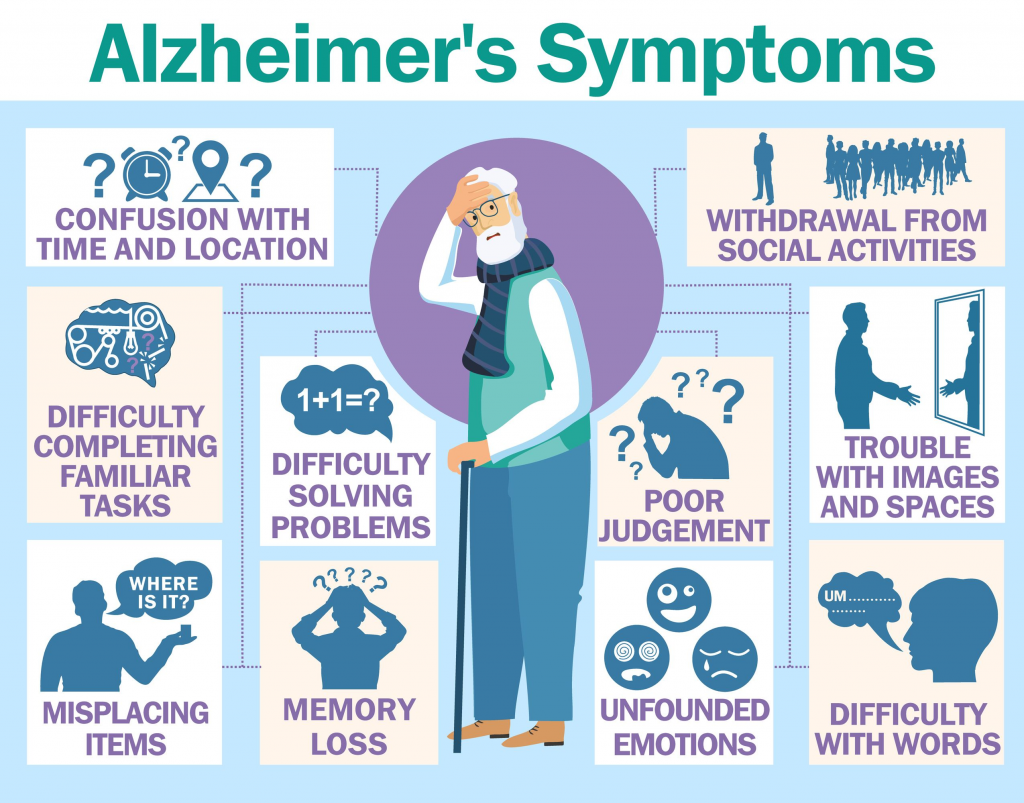
Alzheimer’s disease is characterised by the production of Aβ senile plaques and the aggregation of tau-mediated neurofibrillary tangles. According to recent findings, eliminating amyloid β oligomers and plaques using monoclonal antibodies may stop progression. However, a challenge is the efficient delivery of therapeutic drugs across the Blood Brain Barrier (BBB) for the treatment of central nervous system (CNS) diseases. The BBB is a thin membrane formed by endothelial cells that removes 98% of small-molecule medications and 99.9% of large-molecule therapies for brain diseases, causing drug transport-related issues. The BBB presents a significant impediment to the delivery of medicines to the brain. Yet, the US-targeted microbubble destruction can promote the entry of therapeutic molecules into specific CNS regions, enhancing gene-carrier absorption in damaged brain areas while preventing the loss of normal cells.
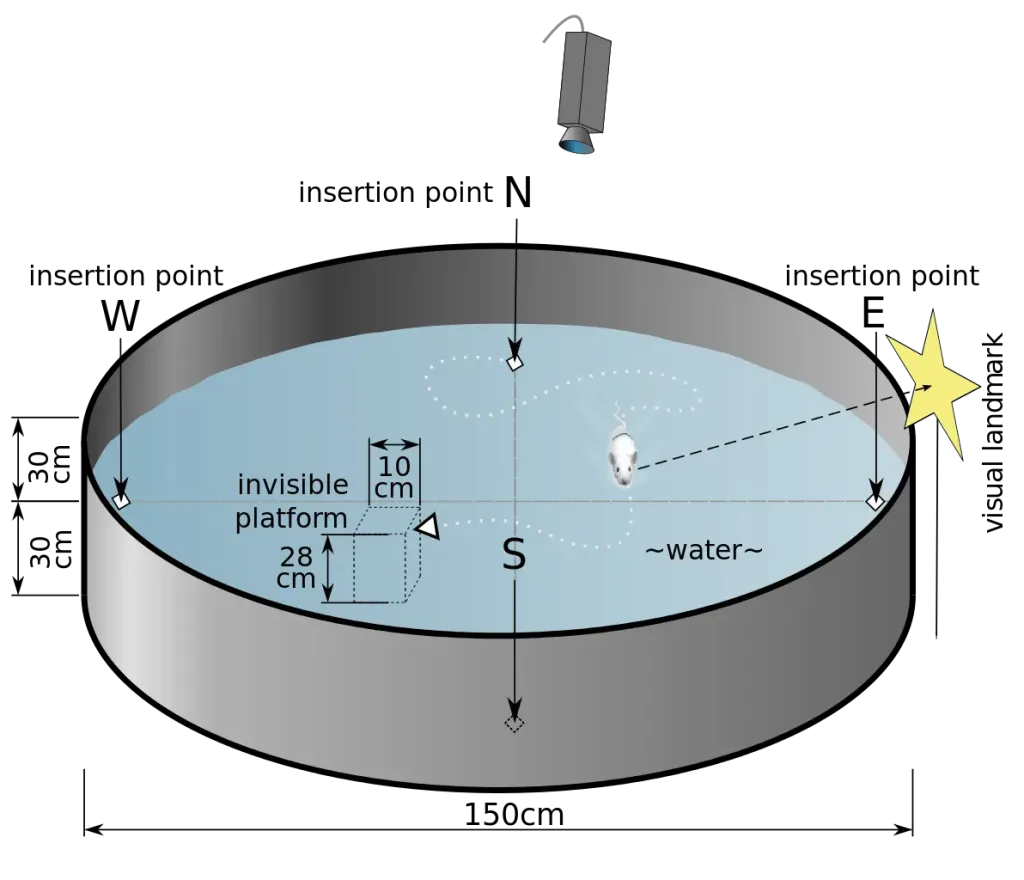
Zhu et al., (2022) investigated the efficacy of US-targeted microbubble destruction (UTMD) in the dual delivery of beta-amyloid (Aβ) antibodies carried by MBs and neural stem cell (NCS) of AD. They used 27 transgenic mice (Tg) and 33 wild-type mice, who were allocated into two groups: control and MB with AB and/or NSCs. The Morris water maze test was used to investigate cognitive and memory processes. As we learned in class, tissue engineering research employs knockout mice, which are a type of Tg. These are genetically engineered mice that receive foreign DNA. The difference between knockout mice and Tg is that the latter has a foreign gene introduced into their gene, e.g., AD. They discovered that the BB opened in Tg mice given a combination of NCS and Aβ antibody UTMD group. Their memory performance and spatial learning improved, and they discovered a reduction in Aβ plaques in the hippocampus and cortex.
A detailed video of how microbubbles work in the brain
In conclusion, the use of MB could open a plethora of solutions to incurable diseases such as Alzheimer’s. However, further research needs to confirm its efficiency. For example, the US successfully destroyed MB, but what debriefs particles? Could it raise any side effects? Furthermore, given that dementia primarily affects the elderly, some individuals may underestimate the importance of discovering a cure for AD. E.B. White did pass away from old age. Throughout my research, I came across the Alzheimer’s Society website, which collects real-life accounts of dementia patients. I’ve noticed that diagnosis is made to one but it affects the entire family. E.B. White’s son would read him his very popular books, to then be asked who the author was. Alzheimer’s is an emotionally and physically draining disorder that affects members of a family, thus treatment is sought to lessen the pain of diagnosed patients.