Recently I read a news article about a man called Adam Castillejo who was cured from HIV by a stem cell transplant he received for a cancer that he had and is still virus free 30 months after stopping HIV medication! This compelled me to research further into this, as I personally would have never made this link.
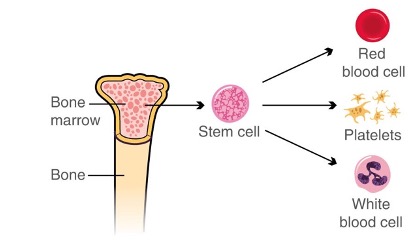
Stem cells are known for their ability to change into specialised cells that later develop to become blood cells, bones, and all human organs. Stem cells are cells produced by bone marrow and utilised to treat many medical diseases and conditions with their potential to repair, replace, restore and regenerate cells. They are most commonly used to replace damaged cells in cancer patients to fight such diseases.
I’m sure almost everyone has heard of HIV, but just to recap, HIV stands for a Human Immunodeficiency Virus that weakens people’s defence against infections and is most prevalent in male homosexual contact. At the end of 2018, it was found that an estimate of 1.2 million Americanshad HIV, with 76% of those being men. To shock you even more, HIV is top 15 for the leading causes of death globally in 2016. Now with that background knowledge of both, have you ever thought that stem cells can cure HIV?
I particularly have never put two and two together, however, with recent news, it is stated that there are currently five people cured of HIV – most of them cured as a result of stem cell transplants. Current research has illustrated that stem cell transplants stop the HIV virus being able to replicate by replacing the patient’s damaged immune cells with specialised donor immune cells that resist the HIV infection. However, this treatment is aggressive and primarily used for cancer patients, and health professionals suggest not using this therapy for those on successful anti-retroviral treatment for HIV.
The primary goal for treating HIV is the clearance of the virus from the body through augmentation of immune responses. For those who don’t know, CCR5 is a receptor that HIV uses to enter cells in the body. Those who are resistant to HIV appear to have two mutated copies of the CCR5 receptor, which means that the virus cannot penetrate the cells. Researchers have suggested the use of gene therapy (gene modification) to target the CCR5 receptor in HIV patients. Researchers are currently developing strategies to cure HIV, with the idea that stem cells are resistant to the virus, the cells produce lower amounts of infectious virus, or the cells specifically target the immune response against the virus.
Previous clinical trials have shown new advances in these stem cell-based approaches to curing HIV, with onein particular demonstrating that large-scale gene therapy trials can be done in a conventional and reproducible way. This efficient way to produce these specialised stem cells is ground-breaking and only further paves the way for a promising cure!
For me, I would have never thought stem cells to be the cure for HIV, or even the fact that this disease is curable with, although very few, survivors. I feel that this topic is very underdiscussed, especially since reading into this field, I have only further enriched my knowledge. New and current emerging information on HIV and gene therapy has laid the groundwork for the potential development of a cure for HIV, however, long-term follow-up is needed.



This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…