Survival of the fittest is a well known theory presented by Charles Darwin. It suggests that organisms who are more adjusted to the environment surrounding them will become more successful in survival and reproduction. Considering this, if you had the opportunity to ensure your child was the cream of the crop, would you take it?
Why was I fascinated by this topic?
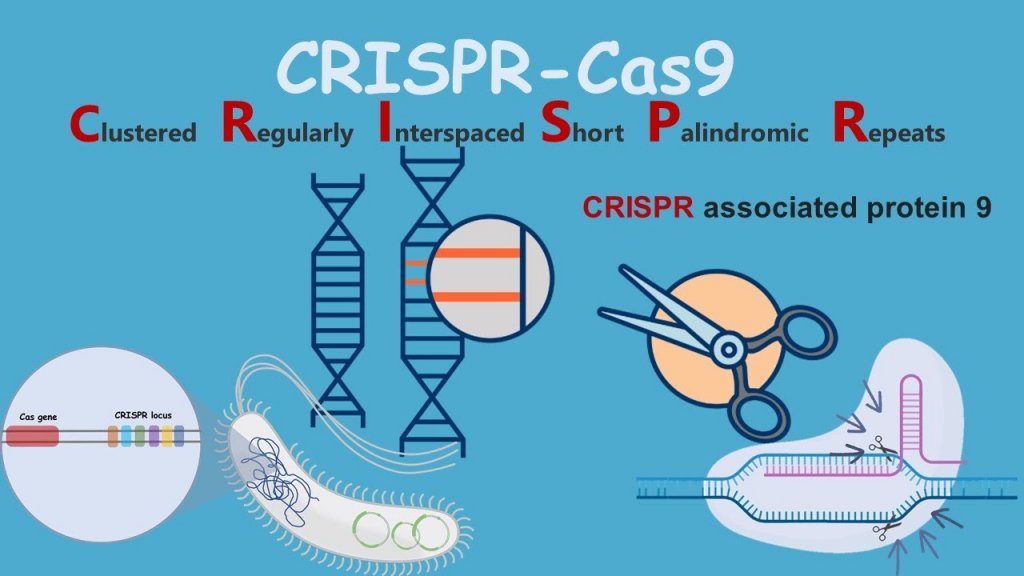
During a recent workshop relating to the law and ethics of replacement body parts, I was fascinated by the debate amongst the group. Specifically relating to ‘Engineering the ‘perfect’ child’, this is a debate brought upon by the altering of genes of an embryo (pre-implementation) using genetic engineering technology: CRISPR. After being split into small groups, with my group consisting of only scientists, it became clear that a lot of our thoughts and feelings towards the subject were very objective, looking purely at the scientific benefit. At the time this view seemed very rational however, after discussing it with some students from the social sciences, our eyes were opened to other perspectives i.e ethical concerns.
At the start of our discussion, I believed this advance in science, namely being able to alter genetics with a desired outcome, could provide life changing techniques to prevent illness in those who are susceptible. It therefore baffled me as to why someone wouldn’t want to beat genetic diseases. For example, being able to remove variations in BRCA1 and BRCA2 genes, which increases a woman’s chance of developing breast or ovarian cancer, where an offspring of parents carrying the gene has a 50% chance of obtaining the harmful mutation from either parent. Upon this case, my initial thought was that there would be elevated stress for the pair that would like to conceive, as they will carry the fear of passing this onto their child. So using this technology was surely a good thing.
After these thoughts, I watched two videos, the first by the economist on the applications of this technology. A banana farmer, James, had his plantation hit with a disease called necrosis that wiped out entire populations of crops. As such, James spent lots of time genetically engineering bananas that withstand this disease, and prevent the fruit becoming extinct. The limiting factor here is societal views of genetic modifications, meaning people weren’t going to buy them. But why?
The problems with CRISPR based genetic engineering
Discovering that this technology could be exploited in multiple ways changed my emotion towards it, I felt uncomfortable. Using this technology for cosmetic purposes, e.g. designing a child as if in a life simulation game seemed unnerving. Firstly, this provides further separation in economic classes. Enabling those who are wealthier to create more ‘ideal’ children to fit in current societal standards. Naturally, this will mean that those who have been conceived with idealistic appearances, will be born into wealthy families, and those who cannot afford to do this, will have natural babies that will inevitably, in time, be seen as inferior.

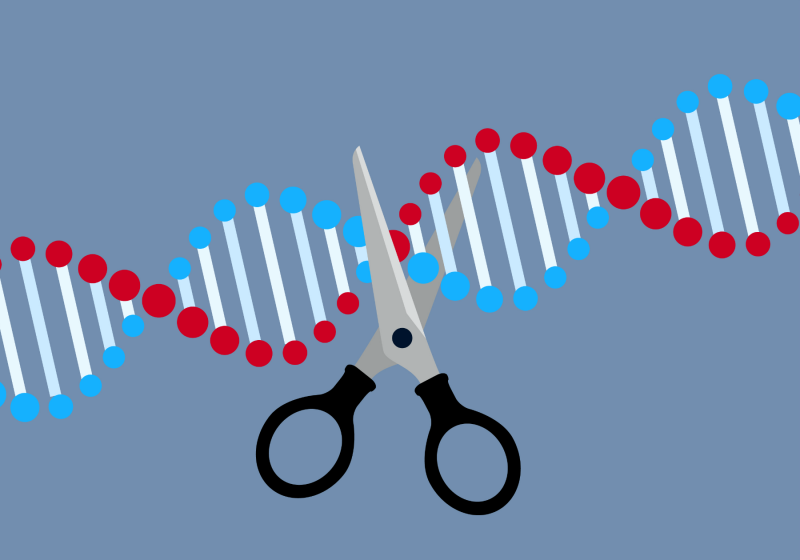
Taking into account both of these possibilities, I decided to further look into this stream of research and watched another video that delves deeper into the CRISPR process and its applications. A statement that stuck out to me in this video was that “.. a door is opened that can’t be closed’. CRISPR is an easy tool, further evidenced by Jennifer Doudna, a biologist who co-discovered how to use CRISPR to edit genes: “Any scientist with molecular biology skills and knowledge of how to work with [embryos] is going to be able to do this,”. Although easy, it doesn’t make it exceptionally accurate. There are possibilities that genes will be edited without intention to. This further poses the question that if an individual had their heart set on a certain child, how would they react to finding out it wasn’t exactly how they planned?
Final thoughts
This debate is far from over, and as time goes on, science will only advance more. It isn’t a case of who is right or wrong but more how we can ensure these technologies are used appropriately. Overall, this debate helped me reflect on my approach to scientific procedures, not only do I have to think about how it might be a great discovery for its intended use, but how it can cause further ethical questions.
Resources mentioned:
Economist video: https://youtu.be/F7DpdOHRDR4
CRISPR video: https://youtu.be/jAhjPd4uNFY
Article on engineering humans: https://www.technologyreview.com/2015/03/05/249167/engineering-the-perfect-baby/



/arc-anglerfish-arc2-prod-pmn.s3.amazonaws.com/public/TQ7UUUQGZBEATPPIT7EWEIWNYE.jpg)









This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…