I was initially intrigued by the concept of Phantom Limb Pain (PLP) because I was fascinated by how someone could experience pain in a body part they no longer possessed. The depiction of PLP in the sci-fi movies I watched when I was younger seemed to be a figment of the imagination; it appeared to be a mysterious occurrence, somewhat fantastical and an element of creative licence adding dramatic effect.
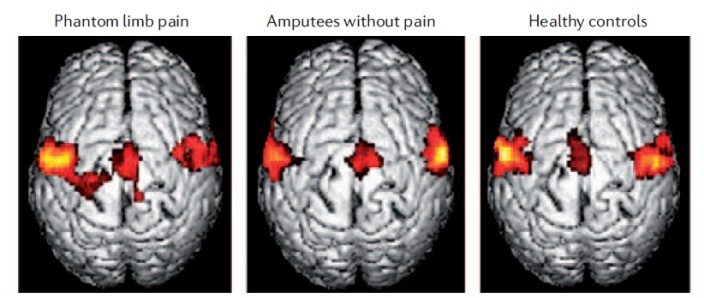
After further research, I discovered that this perplexing phenomenon is real, not make-believe! The basis of PLP although unclear, is suggested to be due to changes in an amputee’s brain organisation; more specifically, alterations in the somatosensory cortex responsible for processing sensory information such as sight and touch, thus affecting the perception of pain sensitivity.
For those who are unaware, PLP can occur within the first few days after amputation; and can persist without intervention. The symptoms vary from the perceived ability to voluntarily move the phantom limbs to intense pain and tingling sensations. PLP treatment is usually with pharmacotherapy, and prosthetic use is considered an adjuvant therapy.
So where do prosthetics come in?
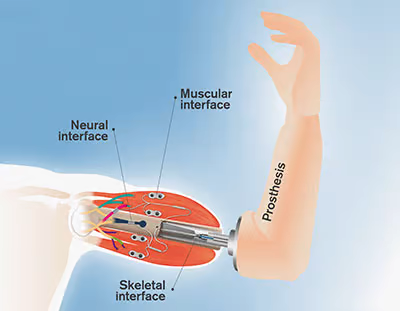
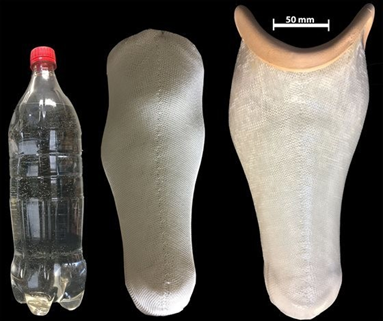
A prosthesis is an artificial device that substitutes for part of the body that is absent due to amputation as a result of a disease or traumatic injury.
Weiss et al. (1999) investigated how increased use of the residual limb by a prosthetic could alleviate PLP by comparing the amount of PLP experienced by upper extremity amputees who wore either the Sauerbruch prosthesis or a cosmetic prosthesis. The Sauerbruch prosthesis allows for the performance of several activities by being connected to one of the muscles of the arm through a surgically created tunnel with cables that operate a rod inserted into the arm, allowing for the contraction and relaxation of the muscle connected to the prosthesis and therefore promotes substantial use of the residual limb. Contrastingly, a cosmetic prosthesis has little functional value and usually leads to the non-use of the affected limb in most individuals who use one. The study concluded that individuals using the Sauerbruch prosthesis have substantially less PLP due to direct motor control of and somatosensory feedback from the prosthetic hand originating in the muscle of the residual limb than those using a cosmetic prosthesis.


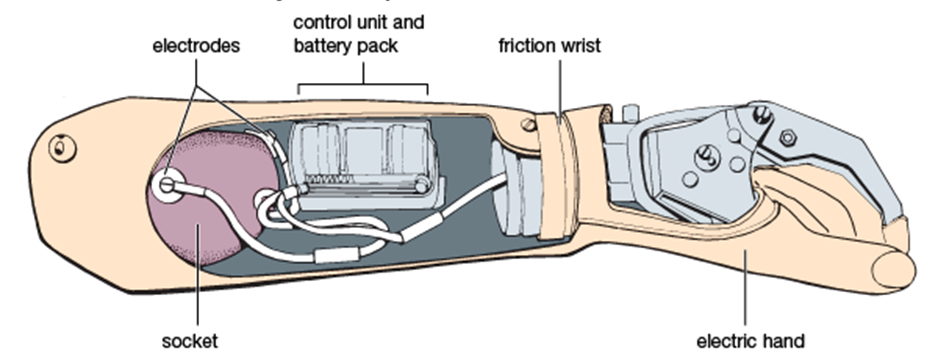
Modern myoelectric prostheses function like the Sauerbruch prosthesis, however, they utilise electrodes in the prosthesis to detect nerve and muscle activity along the residual limb musculature, which triggers motors in the prosthetic to control and produce the movement intended.
Final Thoughts:
The understanding of PLP and prosthetics as an adjuvant treatment allowed me to consider further; whether cosmesis of prosthetics(making artificial limbs look lifelike, similar to the original missing limb) aids the alleviation of PLP, as the somatosensory cortex also processes visual information.
My learning extended to another study suggesting that the correction of body perception may modulate PLP. This hypothesis stems from the prosthetic ownership concept, whereby prosthetic use is experienced as part of the body rather than an attached device foreign to it. This added to my insight into the prosthetic treatment of PLP as the brain combines visual input and direct cortical-somatosensory electrical stimulation by the prosthetic, creating a multisensory illusion that an artificial limb actually belongs to the body, thereby reverting the somatosensory cortex to a healthy state.
Overall, PLP accounts for a significant reduction in the quality of life of amputees; thus, the development of prostheses with somatosensory feedback and a cosmesis effect is a promising therapeutic tool to reduce PLP.
:focal(808x298:809x299)/https://tf-cmsv2-smithsonianmag-media.s3.amazonaws.com/filer/53/c3/53c3b6a3-929b-43f1-bf61-2d2cafbbecca/lacks1.jpeg)







This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…