The Science of Science Blogging: Separating Fact from Fiction
“The greatest enemy of knowledge is not ignorance, it is the illusion of knowledge.”
Stephen-Hawking
Throughout my early scientific career, I have observed that reliable published scientific papers often have perplexing scientific-terminology. So, what’s the solution? Blogs? A form of comprehensible literature, however, they introduce bias. The author is advocating their opinion, providing opportunities for unreliability. Whilst in this blog, I will not directly discredit other authors, I will provide guidance for reading blogs using controversial topics.
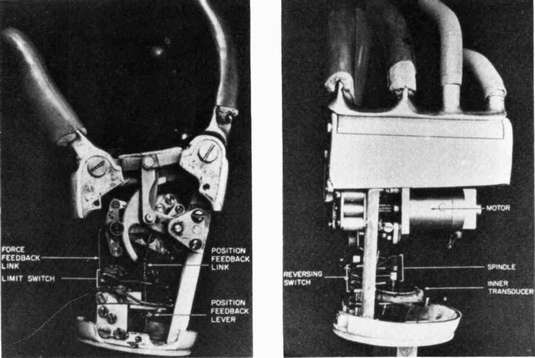
Engineering Prosthetics: A More Accessible World?
We currently have Myoelectric Prosthetics, which use muscles from residual limbs of amputees to control appendages. Advancing technology strives towards fully-integrated prosthetics (requiring only the nervous system to function). I see this concept as enormously advantageous to society, improving the lives of 57.7 million amputees worldwide. I recently watched a video about an amputee called “Johnny Matheny” and I felt captivated by his excitement towards a future where amputees don’t feel disadvantaged.

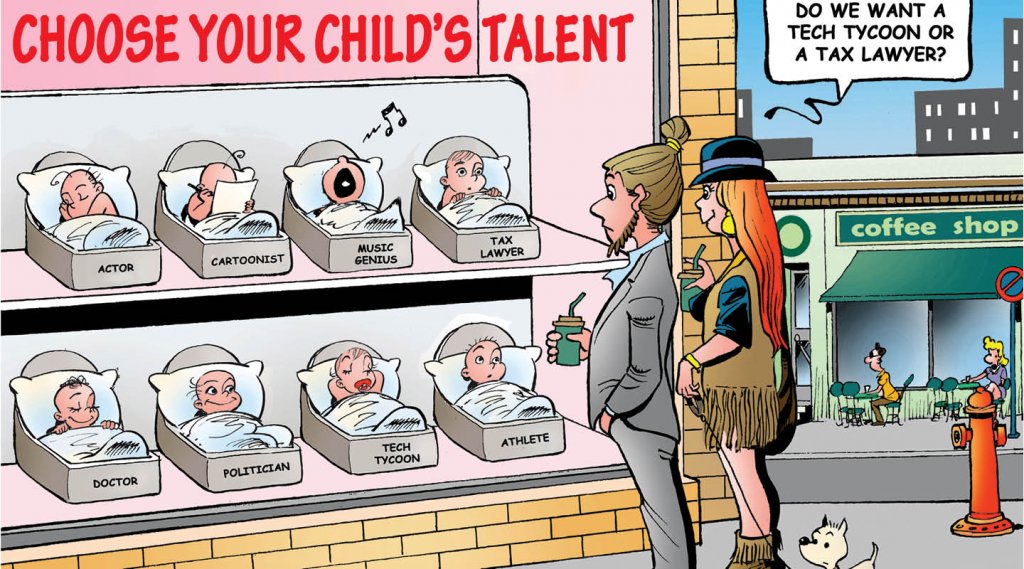
Did my opinion alter yours? The data, case study and emotive language was skewed towards one point of view, however my opinion is more complex. My opinion failed to debate and evaluate the ethical, societal and legal concepts. Ethically speaking, creating a fully functional limb out of carbon-fibre could almost be considered as a weapon (which frightens me) and conversely, the concept could be militarised causing international tensions. Moreover, limb loss occurs in the military hence an unfair expectation to re-enlist as a chimera of man and machine after already losing a limb for their country may occur. Furthermore, I feel as though in events such as the Paralympics, the success of the athletes would be more reliant on the technology of their prosthetics rather than personal skill which I deem as de-humanising our society.
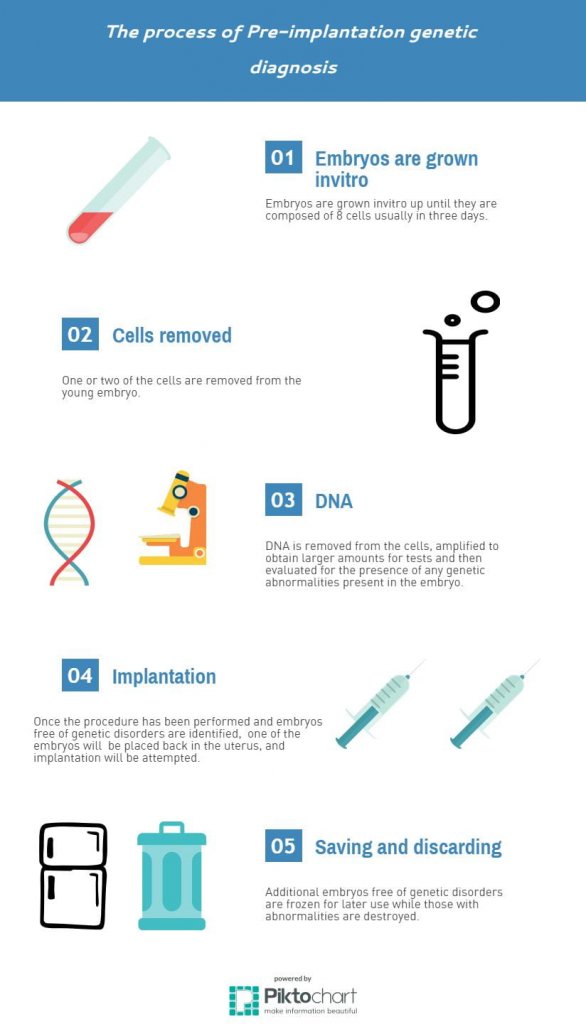
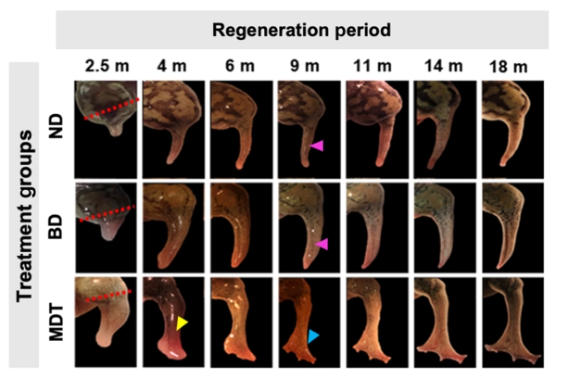
Ethical Considerations of Embryonic Stem Cells: A Delicate Balance
In my opinion, embryonic stem cells should definitely be utilised as they are pluripotent, hence could benefit billions. As an individual with impaired eyesight, the future prospect of replacing damaged photoreceptor cells to cure blindness is attractive to me.
However, my opinion has failed to focus on the ethical opposition. Some element of my moral conscience believes that it’s inhumane to fertilise the egg and then proceed to deconstruct a material that has the capacity to become a sentient being. Aristotle’s eudaimonia virtue ethics valued the preservation of life, and similarly my moral compass burdens me with the thought, should embryonic stem cells be illegal due to lack of embryo consent? “Section-10(2) of the Human Rights Act specifically prohibits involuntary medical or scientific experimentation”, so should this law be inclusive of embryos? Moreover, Jeremiah 1:4-5 says “Before I formed you in the womb I knew you, and before you were born, I consecrated you.” This quote suggests that spiritually, we were pre-determined before the act of egg fertilisation, and hence even though the embryo isn’t sentient, God had a plan for them. As an individual raised as a catholic, I don’t take this quote as literal, but more as a metaphor on the importance of all life. Therefore, I still believe the benefits outweigh the moral dilemmas.
To Conclude…
Overall, I have taken a consequentialist/utilitarian view as I believe the benefits to society outweigh the ethical issues, yet I experience some internal confliction. With blogs, the passion/opinion of the author may be persuasive and result in bias/propaganda. Also, blogs may be oversimplified, hence to form your own opinion, multiple sources must be viewed.
Watch Paul Fairchild justify his use of stem cells:













This is an initially reflective and well researched blog showing how you have chosen to explore the emerging field of…
This is a good attempt at a blog, where you reflect on your recent learning at a lecture/workshop to describe…
This is a fair to good blog, reflecting on your recent learning in some of your modules. You provide a…
This is an engagingly written and reflective blog focussed in general on ethics in medicine. You might improve by citing…
This is a good and well written an presented blog on an original subject - biofilms on implants. You explain…