I have recently had the opportunity to meet a very successful surgeon who specialises in Hip replacement and trauma surgery. Prof. Douglas Dunlop was kind enough to invite me to his clinic where a one hour conversation inspired me to write this blog. He gave me a lot of insight about hip replacement surgery and with that, exactly what could go wrong.
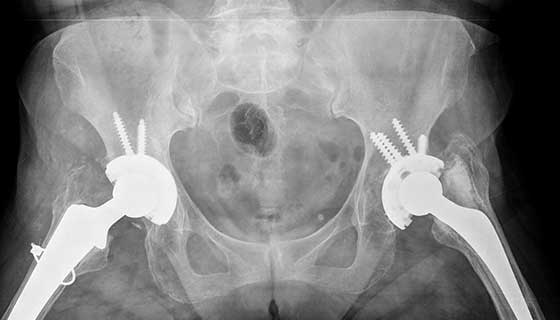
Initially Prof. Dunlop showed me a couple images of hip replacement x-rays, such as the exemplar. One in particular was an image of an anonymous patient, an elderly male who had undergone multiple hip replacement surgeries. Prof. Dunlop and I have discussed why more than one surgery was needed, which leads me to talk about Hip replacement, and it’s potential risks. It might be miss-leading for me to use that title considering it’s impossible to write about every setback, but I will aim to discuss the ones I have learned about.
Going back to the patient. Initially the male had a 3M Capital hip, which due to poor performance lead to revision. Prof. Dunlop explained that the femoral head of the implant became loose in the joint along with the cement holding it together. The friction exerted on the socket lead to osteolysis and screws were needed to keep the implant in the shallow socket. I will not be going into a lot of detail on the 3M Capital hip, but upon further research I have stumbled upon a risk assessment document. It pinpointed that revision was more common in males, and the findings from the report were conclusive; the 3M Capital hips had higher revision rates than other commonly used prosthesis. In addition, with each round of surgery, the hip stem needed to get larger. To make room for a new implant, the femur needs to be reamed. This in turn sacrificed the bone, increasing the risk of fracture, along with loosening of the prosthesis or infection.
Why do hips fail?
I was surprised to hear that the patient had over 3 hip replacement surgeries. On that note its very important to not only think about the failure of the prosthesis, but also why they are initially needed.
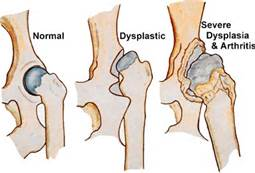
In our discussion, Prof. Dunlop identified the two most common causes of surgery in his patients; arthritis and hip dysplasia.
Hip dysplasia is a medical condition where the hip socket does not fully cover the femoral head. This in turn creates a very shallow socket, which is very susceptible to osteolysis. Friction damages the labrum that lines the joint and can lead to hip labral tear, causing pain and discomfort. Arthritis gives rise to similar symptoms and can have multiple causes.
(MORE) problems with prosthetics.
Wear and tear has a honorary mention on this blog. It seems to be one of the leading culprits for hip surgery, damaging not only the bone, but the implant itself. Below is a list of a couple other things that could go wrong:
- Loosening – causes pain and can lead to an inflammatory response
- Dislocation of the prosthetic
- Tendonitis – inflammation and injury of tendons
- Fractures – example of stiffer hips made of cobalt chrome with 3.4% fracture rate and CPT (Zimmer brand) previously used at Southampton General with a high fracture rate.
Prof. Dunlop also highlighted that often a ceramic head is used in combination with a metal stem for the prosthetic. Many surgeons are now moving away from monoblock prosthetics as the acetabular component cannot be changed.
Where to go from there?
Hip prosthesis may lead to a lot of uncertainty, but just like any other invasive procedure it comes with risks and benefits. I once met a lovely woman called Anne; she has had both her knees and one hip replaced, and yet she has no complaints. In fact she said that the surgery was “life changing”. It allowed her to carry out day to day activities at the age of 87!
Despite ‘all that could go wrong’, it is very important not to overshadow all the benefits that come with prosthesis. The risks can be analysed, prompting researchers and surgeons to develop more successful treatment options and prosthetic joints with less complications. It is fascinating to see what the future of prosthesis may hold!
A large review study demonstrated that hip replacements last 25 years in approximately only 58% of patients.
Centeno-Schultz clinic
This is an excellent blog where you have reflected on your learning and satisfied your curiosity about an aspect of the module by engaging directly with a clinician. You reflected throughout, and it was clear from the narrative how your knowledge and understanding had developed through your interactions.
You could improve by hyperlinking your sources (or referencing them so they are searchable) and by engaging in critical analysis of your first-hand discussions, supporting your conclusions or questioning them by further reading and reference to your sources.