Significance of Tissue Engineering
Whilst protheses are a good mechanism to improve patient quality of life and aid daily function, there remain limitations in which they may not fulfil the needs of the patient.
- They can only provide limited forms of support, meaning they are not appropriate for use with many medical issues
- Requires replacement on a timely basis
- Body often rejects them due to foreign material
Living biological materials may be better suited to meet medical needs – introducing the need for tissue engineering.
Following discussion on the limits of prosthesis, I thought about what biological materials would be structured for longevity in the body.
The Regenerative Nature of the Liver
The liver is the only organ which can regenerate damaged tissue – the organ has the ability to regrow around two thirds of the healthy cells. In line with this, reading led to me an ongoing trial which acts to use the regenerative nature of liver cells in order to help those suffering from end-stage liver disease.
Growing Mini Livers
The emerging medical experimental treatment is titled “Allogenic Hepatocyte Transplantation Into Periduodenal Lymph Nodes”
This entails the use of Hepatocytes, the cells which make up the majority of the liver, which are also allogenic cells, which are sourced from human tissue donors. Using these to try to successfully create an engraftment into the lymph nodes essentially aims to create functioning mini livers in the body!
The purpose of the trial is to help patients diagnosed with end-stage liver disease.
The main objectives of the trial are listed as:
Dosage
Confirming the optimal dose of hepatocytes for the engraftment
Safety
Ensuring the transplantation is safe in the case of any adverse effects
Efficiency
Confirming the engraftments are reducing symptoms of end-stage liver disease
Should we grow Mini Livers?
It is likely that participants will have to take immunosuppressants, as they would for other transplants, to help reduce chance of rejection.
I think that despite the participants potentially having to alter their lifestyle, if the trial is successful than benefits of the treatment would outweigh potential side effects. As end-stage liver disease can cause decreased life expectancy, treatment which counters this should be approached positively. I also believe the treatment would be significant because:
- There is a shortage of liver transplants so treatment may not be feasible
- Increasing liver mass through the transplantation of hepatocyte may be notably beneficial to those with end-stage liver disease
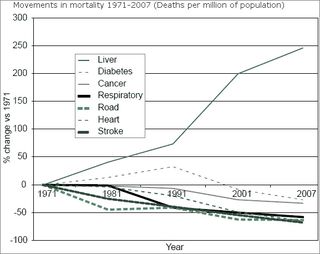
Liver disease is the only major disease in which mortality rates are rapidly increasing
Figure 1: The increase in mortality rates of major diseases
Available at: [https://www.alcoholpolicy.net/2014/10/liver-disease-profiles-highlight-alcohols-role-in-premature-deaths.html] (Accessed: 10/03/25)
I think this trial is significant due to the provision it seeks to give for a widening gap between life expectancy in comparison to other diseases. Whilst many other major diseases have shown decreases in mortality, liver disease has worsened rather than improved alongside other medical advances. I believe the implementation of new treatments is essential to address the imbalance between fatalities of liver disease in comparison to others.
Also, the idea of being able to have lots of mini livers is fascinating!





This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…