What if science could slow down, or even reverse, the unavoidable process of ageing? Recent advances in the field of regenerative medicine and tissue engineering can improve 3D bioprinting which will hold the key to extending human lifespan and improving quality of life in old age. Lab-grown organs to bionic implants, researchers are investigating ways to replace or rejuvenate aged tissues, potentially turning back the clock on the human body (1).

The Science Behind Aging
It is estimated that the average human lifespan is 121 years. Reactive oxygen species depletion, general wear and tear and genetic instability, telomere shortening, mitochondrial genome damage, are the causes of ageing which reduces the lifespan by several years (2).
The ability to repair and regenerate damaged tissues and organs is the foundation of regenerative medicine’s promise. In addition to having the ability to repair some congenital defects, regenerative medicine has demonstrated encouraging outcomes in the regeneration and replacement of tissues and organs (skin, heart, kidney, and liver) (1).
How Engineered Body Parts Can Slow Aging
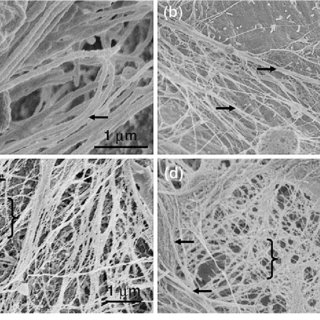
Lab-Grown Organs for Longevity: Researchers are creating bioengineered and 3D-printed organs that could take the role of deteriorating livers, kidneys, and hearts (3).
Artificial Joints and Bones: cartilage-bone tissues can be created (4).
Bionic Eyes and Ears: Second Sight Medical Products created the Argus® II implant, which targets the retina (5).
But while reversing ageing sounds like an exciting prospect, it also raises serious ethical questions. Should we pursue this technology, and if so, how do we ensure it benefits everyone fairly?
The Ethical Dilemmas of Anti-Aging
Technology While the science is promising, reversing aging isn’t just a medical question—it’s an ethical one. Here are some of the biggest concerns:
1. Who Gets Access? – Wealth Inequality & Social Divide: The possibility that only the wealthy can afford anti-aging treatments is one of the main worries. A two-tiered society, where the rich live far longer while the poor age naturally, could result from making reversal ageing a privilege of the wealthy. Fairness and access are called into question: will life-extension technology become just another luxury item, or should it be seen as a human right?
2. Overpopulation & Resource Strain: The world’s population might grow rapidly if people cease getting older, placing tremendous strain on the institutions that provide food, water, shelter, and healthcare. Would populations need to be controlled by societies? In order to balance longer lifespans, would we need to restrict births? A world where people live much longer could have disastrous environmental effects if it is not planned for.
3. Ethical Boundaries – When Should Ageing Stop? Should we reverse ageing even if we could? How does a person’s sense of self and mental health change if they are physically 25 forever? Would the amount of ageing that could be reversed need to be limited by governments? Would society be able to tolerate a future in which no one ever genuinely ages?
Finding a Balance
It’s becoming possible to reverse ageing with synthetic body parts; it’s no longer a science fantasy. But we have to strike a balance between ethical duty and scientific advancement. To guarantee that life-extension technologies benefit everyone, not just a wealthy selects few, careful regulations, fair access, and careful debate are required. While I am excited about the possibilities, I also believe that we should approach these advancements cautiously, ensuring that they serve humanity as a whole rather than creating more social and ethical divides.
The ultimate question is not “can we reverse ageing?” but rather “should we?”
References
1. Dzobo K, Thomford NE, Senthebane DA, Shipanga H, Rowe A, Dandara C, et al. Advances in Regenerative Medicine and Tissue Engineering: Innovation and Transformation of Medicine. Stem Cells Int [Internet]. 2018 [cited 2025 Mar 28];2018:2495848. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6091336/
2. Aging: The Biology of Senescence – Developmental Biology – NCBI Bookshelf [Internet]. [cited 2025 Mar 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK10041/
3. Rando TA, Jones DL. Regeneration, Rejuvenation, and Replacement: Turning Back the Clock on Tissue Aging. Cold Spring Harb Perspect Biol [Internet]. 2021 Sep 1 [cited 2025 Mar 28];13(9):a040907. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8411956/
4. Wu JY, Vunjak-Novakovic G. Bioengineering Human Cartilage–Bone Tissues for Modeling of Osteoarthritis. Stem Cells Dev [Internet]. 2022 Aug 1 [cited 2025 Mar 28];31(15–16):399. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9398485/
5. Stronks HC, Dagnelie G. The functional performance of the Argus II retinal prosthesis. Expert Rev Med Devices [Internet]. 2013 Jan [cited 2025 Mar 28];11(1):23. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC3926652/
This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…