Audio transcript:
The lecture series by Prof Dickinson on prosthetic joints prompted my thoughts on this topic with my tennis interest in Andy Murray and how it has affected close family friends.
The comeback of Murray following his hip resurfacing was astounding. Watching him win the European Open tournament in Belgium post-surgery demonstrated his determination and ability to compete at the highest level.

Murray’s hip resurfacing was done privately and quickly. I will share two stories from close family friends who have had very different experiences on knee replacements.
What is a knee replacement?
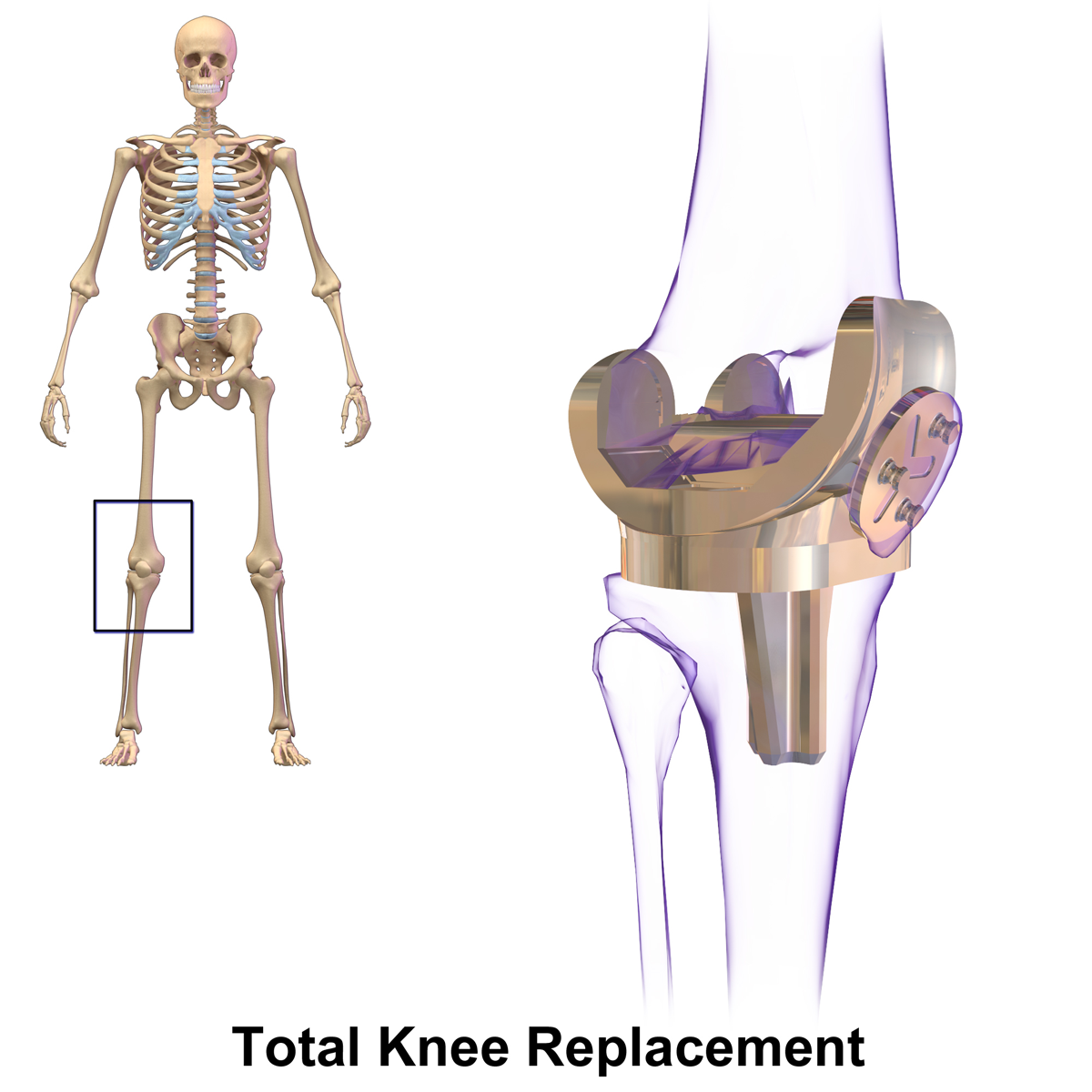
This topic is explained here. The summary is that knee replacements are used to treat pain and stiffness in the joint, usually caused by osteoarthritis. The process involves making an incision in the knee with metal and plastic replacement parts fitted as seen in the image below.
How successful are knee replacements?
A 2020 NHS report found that from over 80,000 patients, 75% responded that they felt much better following the operation with 64% being very satisfied with the results. The success of this treatment is why I feel access to them is so important, but the question of how to make it fair is challenging.
Wait times
The NHS has a very open website called My Planned Care. Taking the University Hospital Southampton statistics accessed on 21/03/2025, in the orthopaedic department the average wait time for treatment was 21 weeks. This led me to read a journal article “Who should have priority for a knee joint replacement?”. The degree of suffering, payment of National Insurance and caring for dependants are reported as the most important factors.
My friends
Ms D went down the private route for her knee replacement and had the operation within three weeks. Before this time, she had put on weight and was withdrawn socially. After the operation, Ms D’s mobility improved, and she resumed frequent international travels.
Ms C suffers from severe knee pain such that she rarely travels far on foot, something that has dampened her usually bubbly spirits. Ms C is opposed to private treatment. She also has a close friend who had a private knee replacement that was infected. Ms C is on an NHS waiting list for knee replacements and is hoping to have the operation in the next few months.
My dilemma
Both people have very different outlooks. My main concern is regarding quality of life. Ms D has now sadly passed away, but she lived ten years with her knee replacement. Ms C is in her late seventies and suffers. I tried to put it to Ms C’s husband in a recent phone call about “Why don’t you consider the private option?”, but it was quickly shot down. If it could be afforded, then the quality of life improvement would be massive, surely it would be worth the money?
Concluding thoughts
Having been a medical student for a couple of years before switching university courses, I have seen first-hand how the NHS system is struggling. I often have a pessimistic view on its survivability in its current form and I see private healthcare as a necessary evil.
Knowing that both suffered greatly, with Ms D having a huge quality of life improvement, makes me uncomfortable with the fact that this could’ve been avoided in Ms C’s case. I find myself feeling regret that Ms C hasn’t put her morals aside for the benefit of her physical and mental wellbeing.
The video below summarises my debate


This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…