In the sensing and sensors lecture, we were shown an example of a prosthetic limb in 2021 with haptics responsive enough that a blindfolded 85-year-old could pick up a hollow eggshell without damaging it1.
This really made me think about the functions you’d need to replicate in a prosthetic arm beyond it being just an appendage for it to fulfill all the roles of the lost limb. I’d only come across haptics being used to extend a user’s ‘self’ in videogame hardware, but with some reflection and research (including on WW2 planes using haptics to forewarn pilots of stalls2) it made sense that the device increasingly becomes an extension of the user with improvements to effective information flow.
So what other sensations are there to improve this link? What other advancements have there been? The sense that immediately comes to mind is temperature, but following that, pain. Pain and discomfort naturally protect us from harm, driving you to avoid potential injury.
In 2018, researchers at Johns Hopkins’ University displayed an electronic synthetic skin called “e-dermis”. A structure of rubber and fabric with sensor “nerve endings” could interact with peripheral nerves of amputees, feeding back curvature and sharpness as “touch” and “pain” respectively. The e-dermis can be implemented on existing prosthetics, enabling users to tell whether they were holding a sharp or smooth object3.
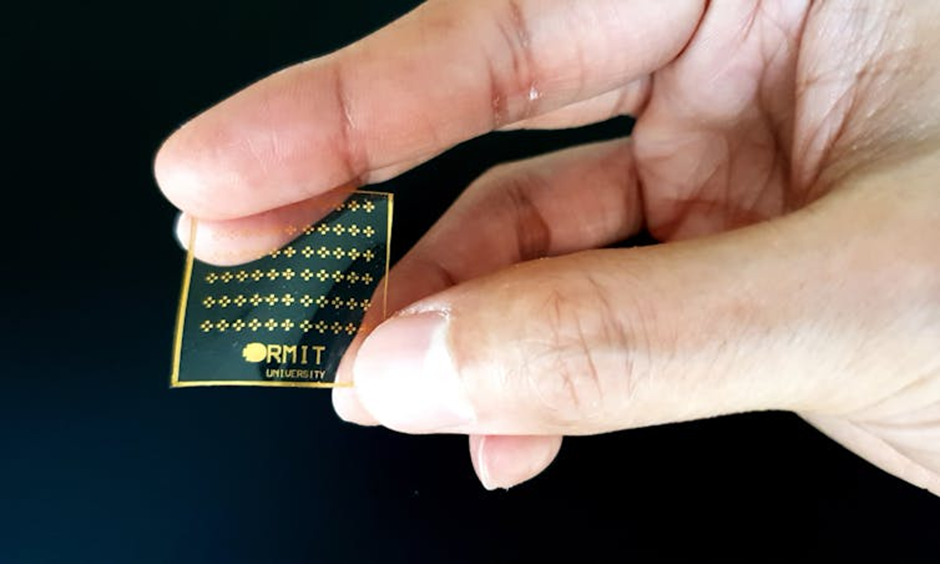
Later in 2020, RMIT University (Royal Melbourne Institute of Technology) developed another electronic synthetic silicone skin. Vanadium oxide’s electronic behaviour changes in response to temperatures above 65˚C, creating a temperature trigger when integrated into the “skin” for pain decision making. Researchers suggested potential applications in non-invasive skin-grafts upon further development, with the “brain-mimicking circuit” having adjustable thresholds to modify sensitivity4.
For anyone reading on these advancements there’s a point that probably stands out though. Do the advantages of simulated pain outweigh the discomfort a prosthetic could inflict on the user when the sensor is on a repairable part?
“After many years, I felt my hand, as if a hollow shell got filled with life again,”-Anonymous principal volunteer tester3.
When implementing the “e-dermis”, stimuli produced by the synthetic skin matched sensations in users’ phantom limbs. Additionally, interaction with peripheral nerves is increasingly well documented to reduce phantom limb pain5,6,7. If reactive pain and sensory feedback can reduce persistent phantom limb pain in amputees, improving brain body mapping for prostheses, the very pain and discomfort we want to avoid could act to unify prosthetic and person.
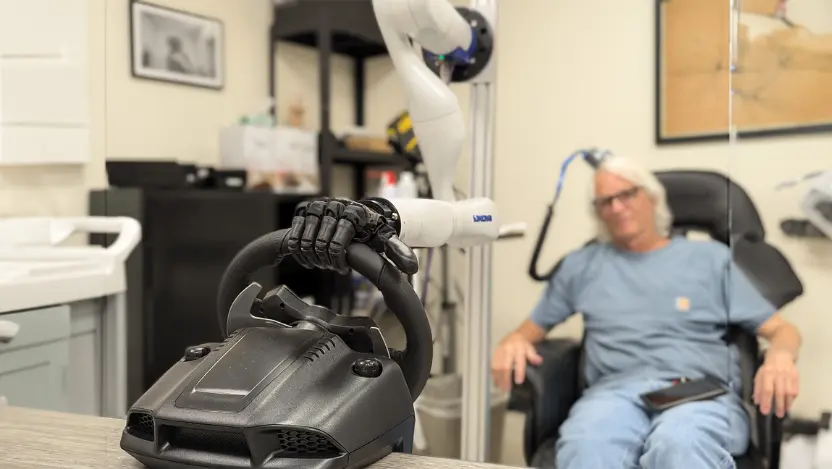
I was also curious what advancements in sensory prosthetics could do for those paralysed by extension. A 2025 study by researchers at the University of Chicago8 worked with individuals with spinal cord injuries. Electrodes were implanted into the sensory and motor regions of the brain, allowing not only control of a robotic arm and hand, but sensation through it. Subjects could feel edges, shapes and movement through their connection to the robotic arm.
Amazingly, subjects had such good control of the limb they could even drive cars (in simulation).
The development of sensation in prosthetics is so much further than I realised, where else could these technologies go? Where else might they end up? If pain, touch, and temperature feedback can be integrated into artificial limbs, could future developments allow individuals to experience a completely artificial yet fully sensory body?
References
- 1 Wong, W. G., 2021, Bionic Hand Provides Strength and Haptic Feedback, Medical Design, Machine Design, available at: https://www.machinedesign.com/medical-design/video/21174228/bionic-hand-provides-strength-and-haptic-feedback accessed 26/03/25
- 2 Loftin, L. K., Jr. (1985). Quest for Performance: The Evolution of Modern Aircraft (NASA-SP-468). NASA Scientific and Technical Information Branch.
- 3 Lunday, A. (2018, June 20). New “E-Dermis” Brings Sense of Touch, Pain to Prosthetic Hands. Johns Hopkins Biomedical Engineering., available at: https://www.bme.jhu.edu/news-events/news/new-e-dermis-brings-sense-of-touch-pain-to-prosthetic-hands/ accessed 25/03/25
- 4 Lacour, S. P. (2020, August 17). Pain-sensing electronic silicone skin paves the way for smart prosthetics and skin grafts. The Conversation. available at: https://theconversation.com/pain-sensing-electronic-silicone-skin-paves-the-way-for-smart-prosthetics-and-skin-grafts-145386 accessed 25/03/24
- 5 Graczyk, E. L., Resnik, L., Schiefer, M. A., & Tyler, D. J. (2023). Peripheral nerve stimulation enables somatosensory feedback while treating phantom limb pain: Long-term usability and satisfaction. Brain Stimulation, 16(5), 1302-1311. https://www.sciencedirect.com/science/article/pii/S1935861X23017618
- 6 Dietrich, C., Nehrdich, S., Seifert, S., Asper, R., Miltner, W. H. R., & Weiss, T. (2012). Sensory feedback prosthesis reduces phantom limb pain: Proof of a principle. Neuroscience Letters, 507(2), 97-100. https://www.sciencedirect.com/science/article/abs/pii/S0304394011014807
- 7 Dietrich, C., Nehrdich, S., Seifert, S., Blume, K. R., Miltner, W. H. R., Hofmann, G. O., & Weiss, T. (2018). Leg prosthesis with somatosensory feedback reduces phantom limb pain and increases functionality. Frontiers in Neurology, 9, 270. https://www.frontiersin.org/articles/10.3389/fneur.2018.00270/full
- 8Marasco, P. D. (2025). Navigating the complexity of touch. Science, 387(6731), 248-249. https://www.science.org/doi/10.1126/science.adu7929


This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…