I recently saw an article about lab-grown meat and how it soon may be coming to UK supermarkets. In fact, cultured meat has been used in dog food since February this year, and in 2020 Singapore allowed cell-cultured meat for human consumption1. However, its use in our food is still awaiting approval by the FSA.
How is meat grown in a lab?
Lab-grown meat, also known as cultured or cultivated meat, is meat developed from a culture of animal cells instead of being farmed from slaughtered animals.
There are four main steps involved in its production2:
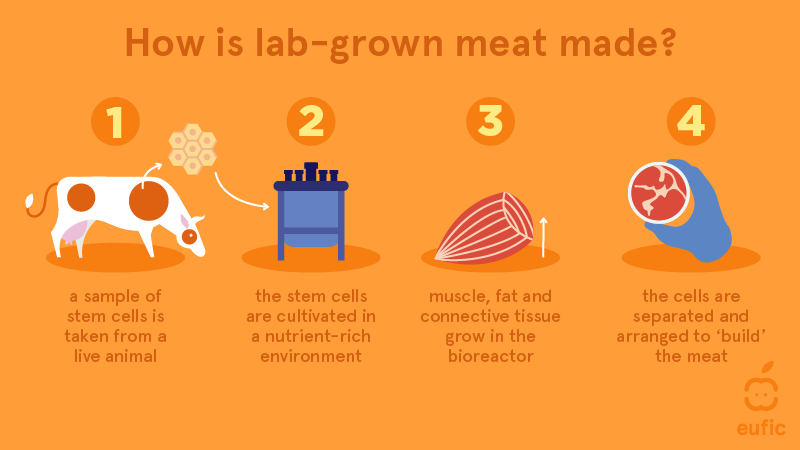
- A stem cell sample is taken from a living animal (e.g. embryonic stem cells or skeletal muscle stem cells: myosatellite cells3)
- These stem cells are put in large bioreactors which contain culture media that creates a favourable environment, one similar to the host animal’s body. These culture media also provides nutrients that the stem cells need for growth.
- The culture media is then changed to a provide a different environment, one that allows the stem cells to differentiate into muscle, fat and connective tissue.
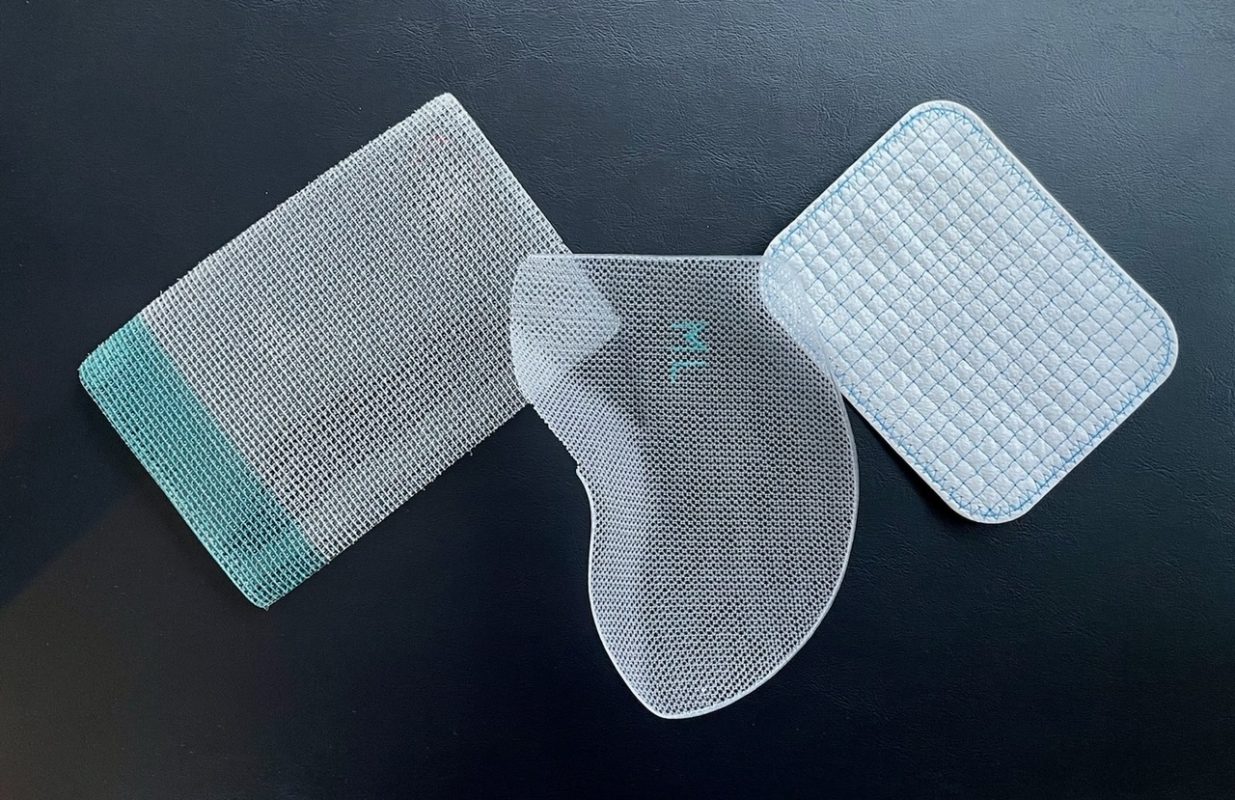
- These different types of cells are separated and used in scaffolding: where the meat is “built” on an edible scaffold (made of collagen and gelatin4) that provides support for the meat cells. This allows them to arrange themselves in the correct way to create the desired meat shape, e.g. minced meat or a steak. The scaffold also provides more nutrients for the cells to further differentiate and make the correct tissues.
Why use cultured meat?
Firstly, growing meat in a laboratory means that animals won’t need to be raised and slaughtered for their meat. This presents benefits like less space and resources being used, as large amounts of animals won’t need to be farmed. A more sustainable method of meat production is beneficial to the environment, especially due to current concerns about climate change caused by, for example, deforestation to make space for herding. Decreasing the amount of animals slaughtered also means that animal rights and welfare will improve, and people who don’t eat meat due to animal cruelty might choose to reintroduce meat into their meals (which is important for a healthy, balanced diet).
Since this meat is grown in controlled laboratory conditions, the risk of parasites, diseases and other pathogens is lowered as the environment the meat is grown is heavily regulated. Common issues such as parasites or bacteria (E. coli, salmonella) could be avoided using cultured meat.
Drawbacks
Studies show that although cultured meat will reduce methane emissions due to cattle farming, its production could contribute to CO2 emissions over a long period. Cultivated meat also requires a large amount of energy, potentially contributing to greenhouse gases if renewable sources aren’t used5.
Personally, I think lab-grown meat does have a role in the future of food as it could also be modified to contain less saturated fats and be overall healthier. However, a large number of people will try to avoid it due to doubting its safety or having a preference that “real” meat tastes better.
References
- Rowlatt, J. (2025). Lab-grown meat goes on sale in UK dog food. BBC News. [online] 9 Feb. Available at: https://www.bbc.co.uk/news/articles/cwy12ejz0mwo.
- Eufic (2023). Lab grown meat: how it is made and what are the pros and cons. [online] www.eufic.org. Available at: https://www.eufic.org/en/food-production/article/lab-grown-meat-how-it-is-made-and-what-are-the-pros-and-cons.
- Swartz, E. and Bomkamp, C. (2022). The Science of Cultivated Meat. [online] The Good Food Institute. Available at: https://gfi.org/science/the-science-of-cultivated-meat/.
- Seah, J.S.H., Singh, S., Tan, L.P. and Choudhury, D. (2021). Scaffolds for the manufacture of cultured meat. Critical Reviews in Biotechnology, 42(2), pp.1–13. doi:https://doi.org/10.1080/07388551.2021.1931803.
- Lynch, J. and Pierrehumbert, R. (2019). Climate Impacts of Cultured Meat and Beef Cattle. Frontiers in Sustainable Food Systems, 3(5). doi:https://doi.org/10.3389/fsufs.2019.00005.
This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…