Is the promise of xenotransplantation worth the potential ethical dilemmas it presents?
During an anatomy workshop in my biomedical engineering module, I observed cadavers and human organs donated for medical education. But as I examined them, I thought about how many of these individuals had died not from old age, but because they couldn’t receive a transplant in time. According to NHS Blood and Transplant, there are about 7,500 people on the UK transplant waiting list. Last year, over 415 people died waiting for a transplant. [1]
How does Xenotransplantation work ?
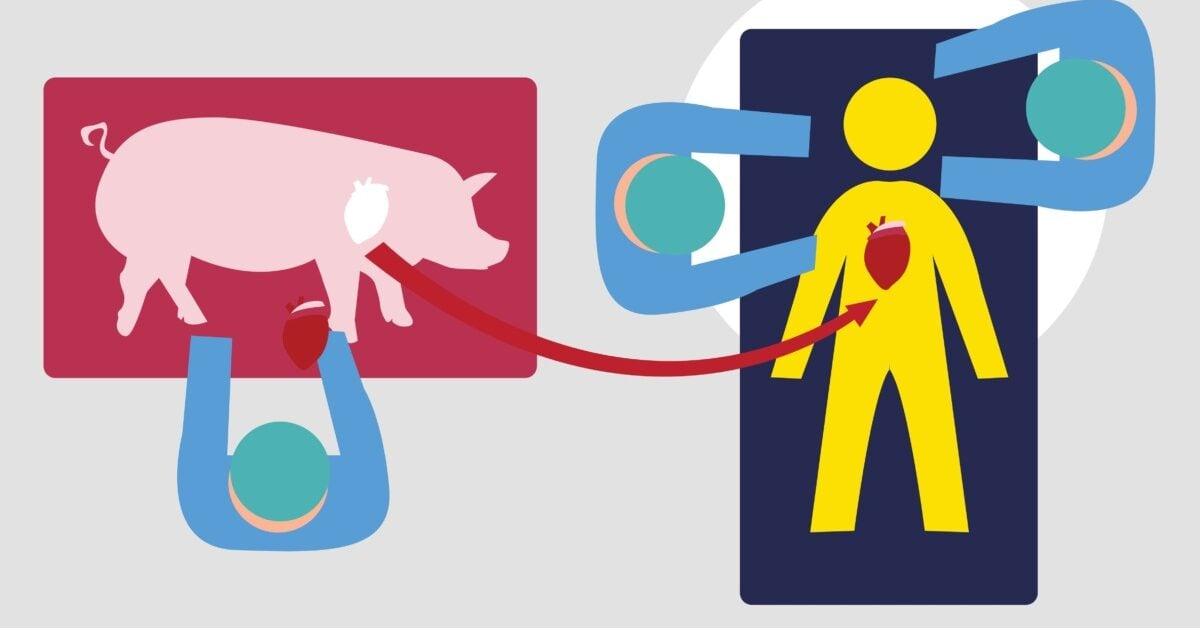
Xenotransplantation involves transplanting animal organs or tissues into humans. Advances in gene editing, like CRISPR, allow scientists to modify pig DNA to improve organ compatibility.As far as research goes, pigs are currently considered the most ideal donor animal hence, it will be the main consideration in this blog.
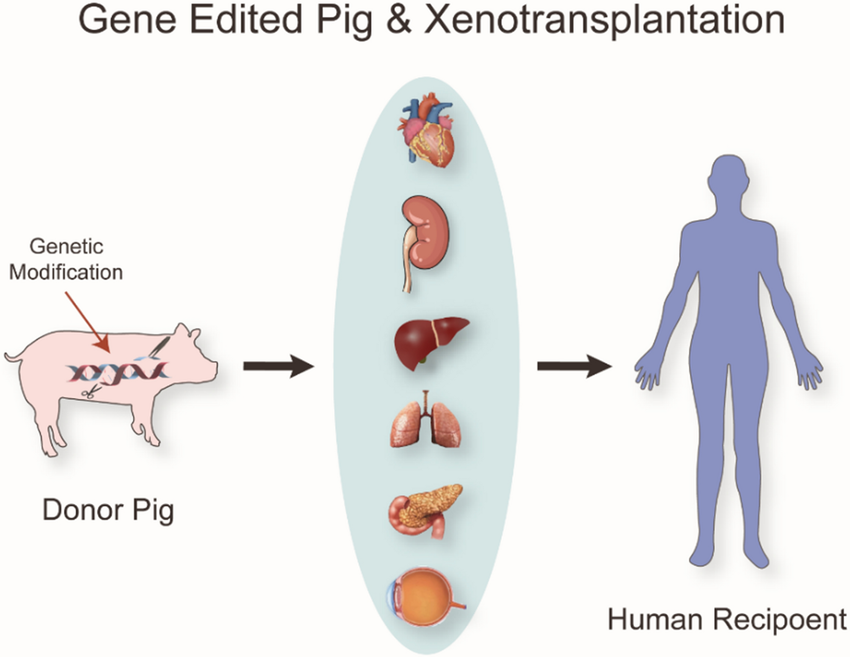
In 2022, the first xenotransplant was carried out on a 57-year old patient who received a pig heart and survived for 60 days after the procedure. Despite his death, the case provided valuable insights into medication, immune response, and organ testing requirements. [2]

However, regardless of all the information learnt from the case, does the fact that we can intervene, mean we should ?
Ethical Concerns
1.A major ethical concern is that using pigs to grow organs contradicts practices for animal welfare that prioritise their behavioural and psychological needs. Unlike farmed pigs used for meat, they are genetically modified and kept in sterile conditions with strict infection-control measures, preventing natural behaviours. They undergo artificial insemination and frequent blood and tissue sampling, often requiring restraint. If used for multiple transplants, they may endure repeated surgeries, causing distress to these highly intelligent animals. [4]
-> However, some may argue that if we are already breeding animals for food, is using them to save human lives worse? I think from a utilitarian perspective, the fact that we already kill animals for meat doesn’t justify using them for their organs as well—especially when they endure harsh conditions beyond just being slaughtered.
2. A major concern with xenotransplantation is the risk of zoonotic diseases like porcine cytomegalovirus in pigs where animal-to-human transmission could cause widespread harm, even a pandemic.
-> From a consequentialist standpoint, this risk could outweigh potential benefits xenotransplantation offers, presenting it as ethically wrong solely based on its consequences. I support this argument because while xenotransplantation could save lives, the potential harm undermines its purpose, as the lives saved may be offset by those put at risk.
Societal/Behavioural Concerns
Even if xenotransplantation becomes routine, will society accept it ?
There is something unsettling about the idea of merging human and animal biology. Some may feel dehumanised, experiencing the transplanted organ as “foreign” or unnatural. While these are valid concerns, if the consequence is loosing your life to a lack of organs, then I would argue that these considerations are manageable.They can be dealt with after receiving the organ through therapy and time. [3]
Additionally, the use of pig organs may be frowned upon by certain religions such as Islam as they are considered forbidden because of their “impurity”. As a result, the transplantation of a pig organ into a Muslim could be seen as violating religious principles and could lead to significant psychological and spiritual discomfort.
Conclusion
While xenotransplantation offers hope, I think there are many ethical considerations such as the transmission of diseases and harm caused to animals that mean we shouldn’t rush into considering it as a solution to the lack of organs for transplants.
References
- NHS. Organ Donation and Transplantation [Internet]. NHS Blood and Transplant. 2022. Available from: https://www.nhsbt.nhs.uk/what-we-do/transplantation-services/organ-donation-and-transplantation/
- Kozlov M. Pig-organ transplants: what three human recipients have taught scientists. Nature [Internet]. 2024 May 17; Available from: https://www.nature.com/articles/d41586-024-01453-2
- Anderson M. Xenotransplantation: a bioethical evaluation. Journal of Medical Ethics [Internet]. 2006 Apr 1;32(4):205–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2565783/
- Rodger D, Hurst DJ, Bobier CA, Symons X. Genetic disenhancement and xenotransplantation: diminishing pigs’ capacity to experience suffering through genetic engineering. Journal of Medical Ethics. 2024 Feb 23;50(11):jme-109594. Available from : https://jme.bmj.com/content/50/11/729

This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…