After learning about prosthesis (replacing a body part or joint) and orthosis (external support promoting healing) I reflected on my own experience. I had a Le Fort I osteotomy, a surgery to reposition the upper jaw. This doesn’t fit either prosthetic or orthosis categories, but is somewhere in between. I knew metal implants were used for this, but hadn’t considered why or how they work.
The best person to learn from was the surgeon himself, so on my previous visit I interviewed with questions based on topics discussed in the lecture:
Me: What material was used in the metal implants and why?
Surgeon: Medical grade titanium, because its biocompatible
Me: How was the metal implanted to hold the jaw?
Surgeon: There are two stages. Primary stability is done in surgery, it’s the tightening of screws into the bone and then you find the bone grows in the threads of the screws and will grow in and over and around the plates, osteointegration it’s called and that’s the secondary stability
Me: How does it change for different sizes and shaped jaws?
Surgeon: There’s a website here, you can even find the whole guide if you want about all the screws they make and where they use them, different plates, different sizes. So, in the face depending on how much load it has to take you change how thick the plates are.
The website mentioned, which allowed me to visualise how the implants were used:
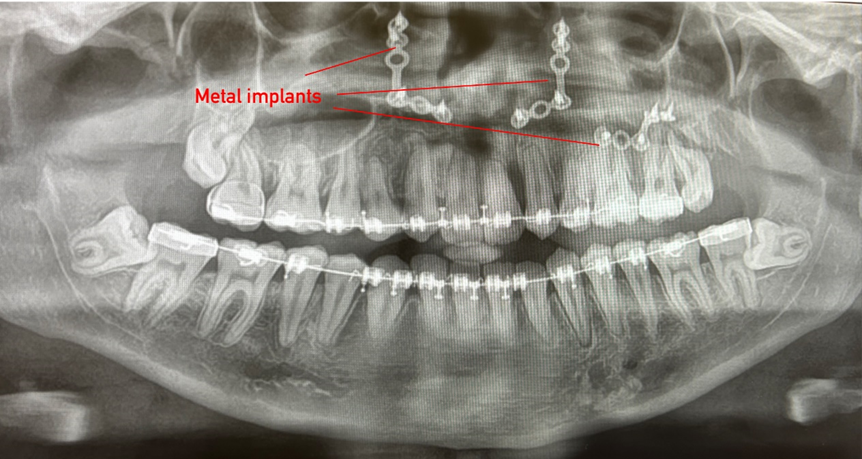
He provided me with my x-ray, showing exactly how the implants are positioned:
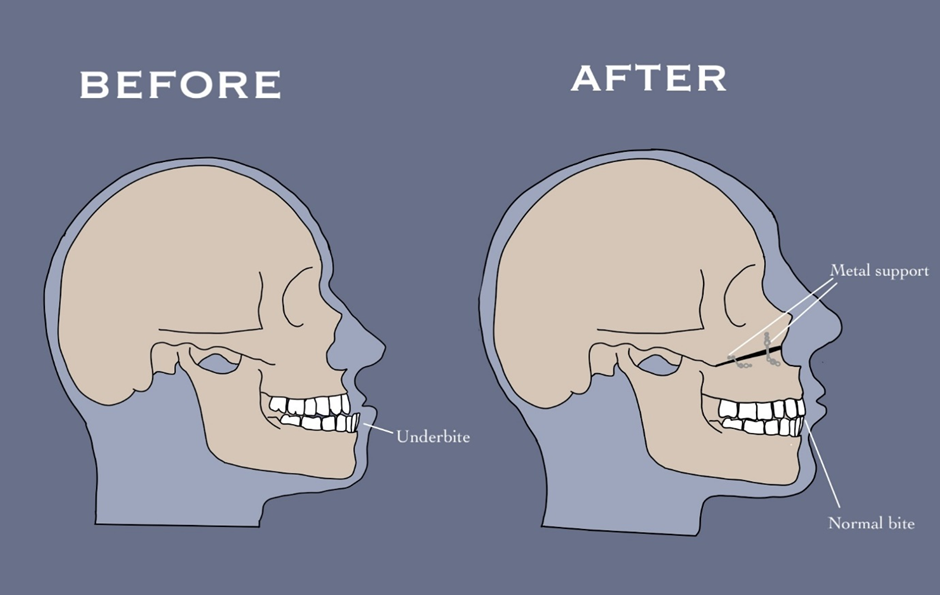
The interview, the website and x-ray gave me a deeper understanding of the role of the metal implants. This led me to create this image, showing how the implants are used:
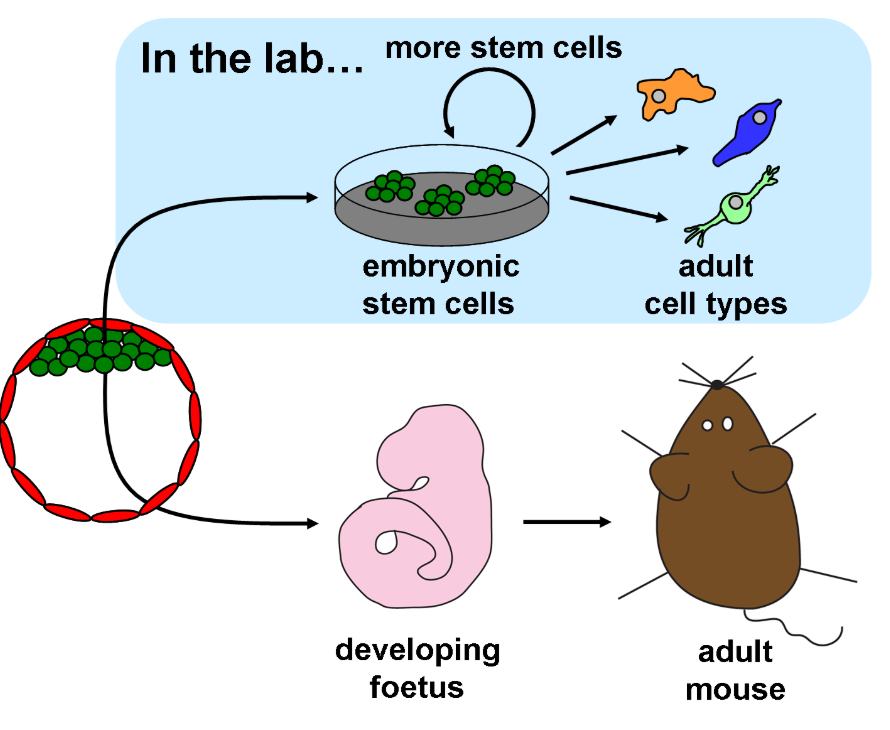
The interview revealed similarities between facial implants and joint replacements, particularly the porous material that I observed in the practical, which allows bone to grow into to stabilise.
Although biomedical engineers design implants to reduce failures, they do occur due to infection, breakdown between implant and bone, and migration of implant. The lecture on this topic made me curious if the same was true for metal implants in the face.
Further reading showed in a study of 485 orthognathic cases, 93 complications were recorded, including failure of fixation, requiring re-intervention (Zaroni et al. 2019). This made me reflect on the ethical considerations when offering this surgery. Unlike prosthetics, which are needed due to pain, orthognathic surgery, is often for aesthetics and ease of eating, both of which are not essential. This raises an ethical dilemma: if not needed, is it worth the risks, even if minimal?
The legal and ethical solution to this is informed consent. This video helped me understand what this actually entails:
I felt the NHS definitely achieved this in my case by repeated discussions over several years. However, I believe knowing the risks doesn’t compare to experiencing them. Something I found extremely useful before my surgery was finding others on social media who had had the same or similar procedures. It showed me the reality of recovery and possible complications. I believe informed consent could be improved by sharing first-hand experiences so I designed a template for a website which would facilitate this.
This would allow more in-depth discussions on what the recovery process is like and how other people experienced complications, rather than just the surgeons’ perceptions. Personally, the minimal risks were worth the outcome, but seeing others who had same procedure helped me make a truly informed decision.


This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…