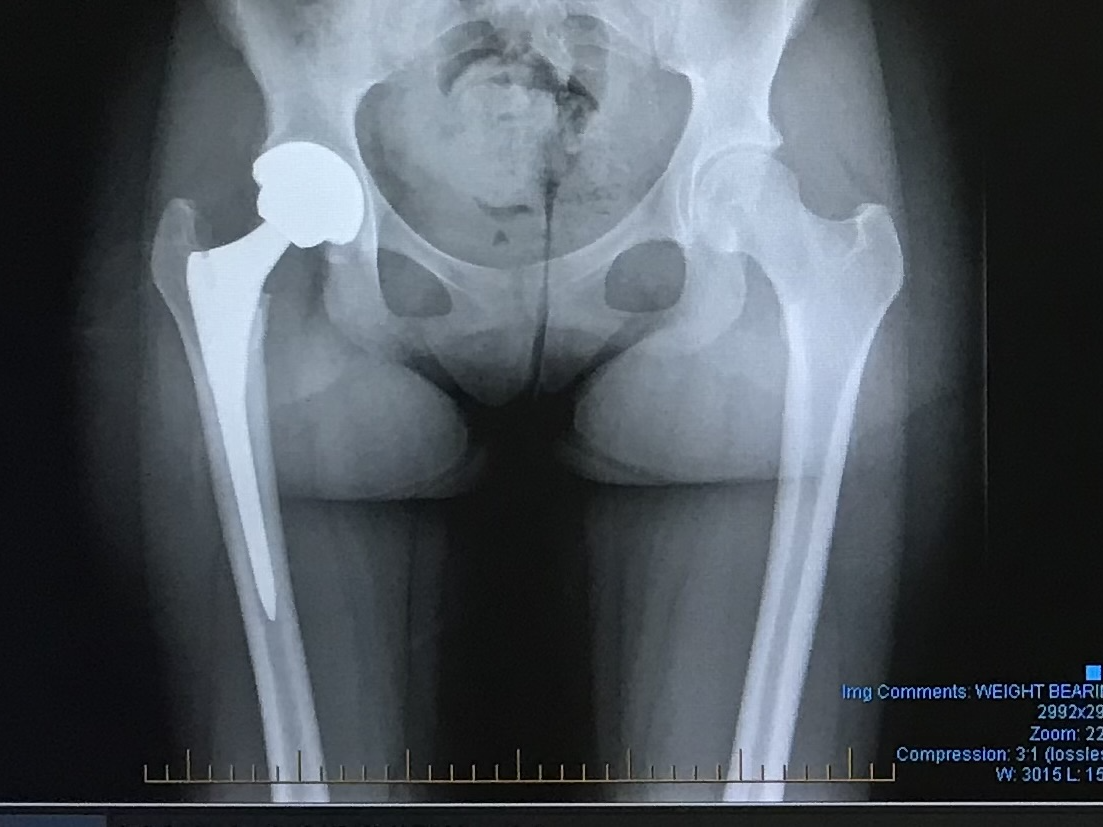
From the perspective of someone who always found the human body intriguing, I never expected my own to become the subject of my fascination. Replacement joints helped make me feel 16 again and I could not imagine being told there was nothing that the doctors could do. This as well as the prothesis lecture by Alex Dickinsons guided me to look into the different types of surgery’s, how long they last for, and the statistics behind young patient joint replacements?
Joint replacements: What are the different types?
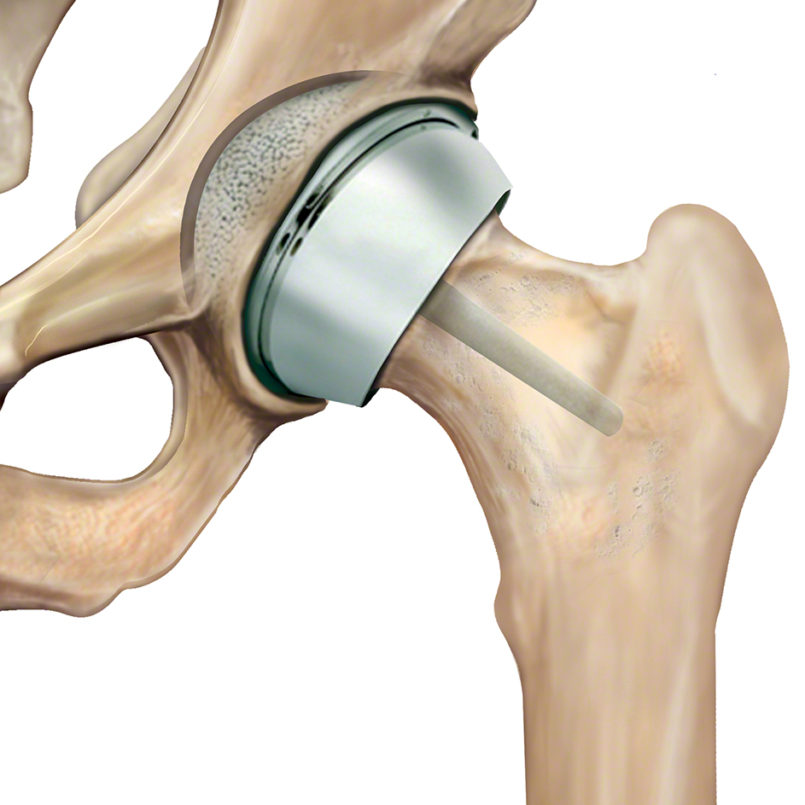
Total Hip replacement: This procedure involves the removal of the femoral head and the cartilage that lines the socket, replacing them with a metal implant that extends into the femur and a plastic lining that is placed into the socket. The implants have three types: metal-on-plastic, ceramic-on-plastic, and ceramic-on-ceramic, each with their own advantages. Additionally, hip replacements can be cemented or uncemented, depending on the patient’s needs.
Hip resurfacing: This is a procedure that occurs when the femoral head is trimmed and capped with a smooth metal shell. This is an alternative to a total hip replacement, recommended for younger patients. This is due to less damage occurring to the bone, preserving bone quality, and increases levels of activity when compared to a total hip replacement.
Advancements in hip replacement surgery: A personal perspective…
Due to experiencing a full hip replacement, I was inquisitive to see the procedure from a surgical point of view. This prompted me to reach out, which provided me with the opportunity to watch a total hip replacement surgery. This was very educating and I found it crazy that patients now experience this with only a sedative and nerve block as well as usually leaving hospital after a day. When I had my hip replacement I was fully sedated, had a nerve block, and stayed in hospital for five days. With my surgery they cut through the glute muscle, whereas with the surgery I saw they moved the muscles out of the way. This can, and has sped up recovery time. For there to be such a change in 5 years, it has made it clear that medicine is always advancing, so why should the age range for a procedure not change?
Why is there usually an age requirement for hip replacements?
The reasoning behind the lack of young patients with hip replacement was due to the lifespan of a prothetic joint, meaning patients may need the replacement revised later in their life. Only so many revisions can occur due to the bone quality. This means that there is only a certain amount of replacements you can have. typically the younger the patient the more replacements needed. However due to the materials used lasting for longer than ever more young patients are able to get replacement joints.
This led me to look into patients with hip replacement and the statistics for young hip replacements, in April 2021-March 2022 for every 100,000 hip replacements 0.8 were aged 10-14 and 3.1 were aged 15-19.
My Thoughts…..
Hip replacements are designed to help people stop being in pain, so why are we preventing that? My hip replacement was the best thing to happen to me and I am so much happier for it. I think that hip replacements should be offered to younger people when needed. People should not be told they are too young to receive medical treatment!

This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…