Can they swing from a thread? No, but they can produce them!
Several years ago, in my GCSE biology class, I first encountered the concept of gene editing and transgenic animals. Since then, I have become very interested in medical devices and biomaterials. Spider goats perfectly combine these topics and pave the way for potentially revolutionary advances in medicine and healthcare.
Spider Goats
Spider goats appear to be completely regular goats at first glance. However, they have a secret superpower: the ability to produce the spider silk protein in their milk!
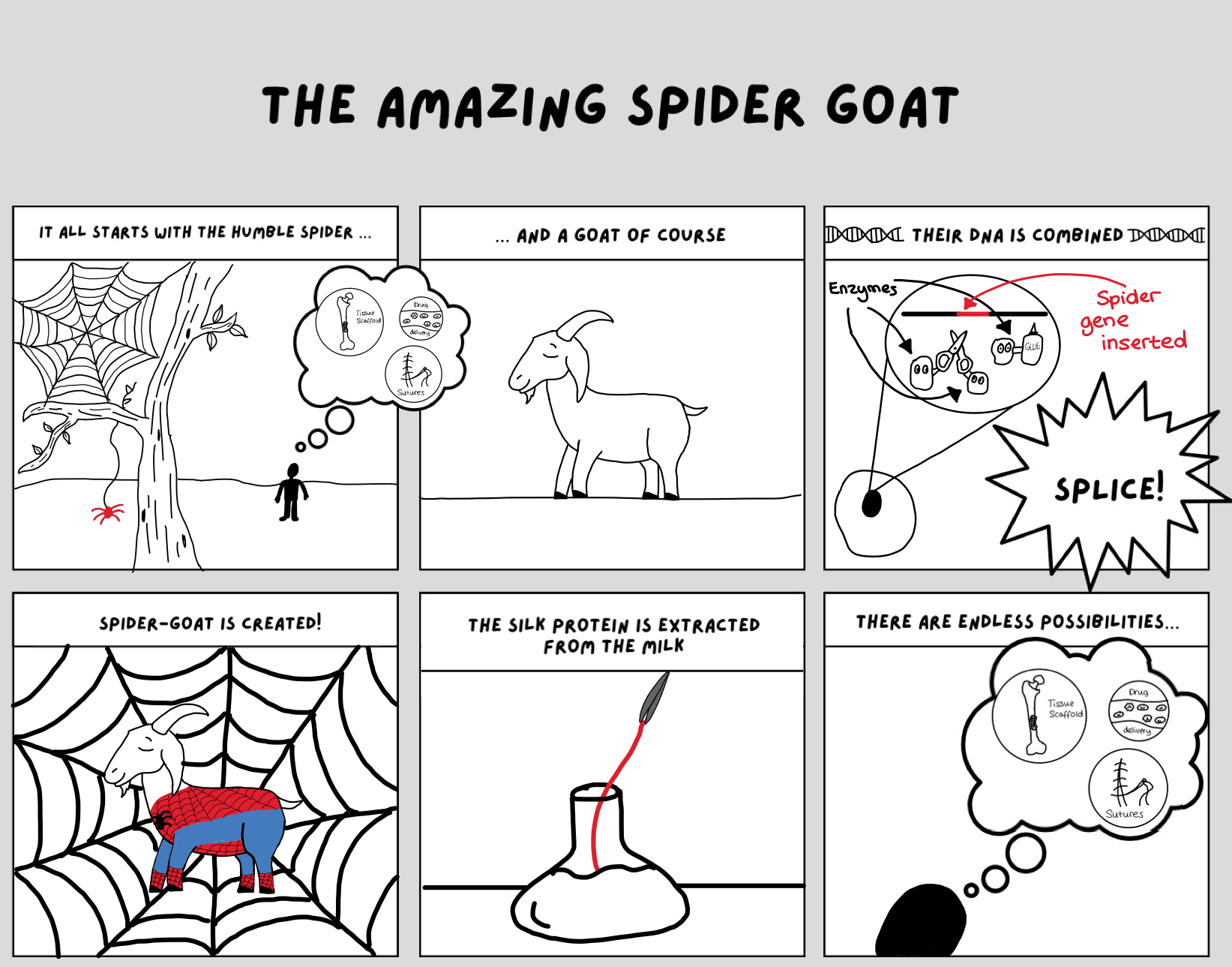
How are they made?
There are various ways to produce transgenic animals. The way it was originally achieved in spider goats was by taking some skin cells from the goat and inserting the gene from the spider that creates the silk protein into the nucleus. The nucleus could then be removed from the skin cell and put into an egg cell, which was then implanted into a goat. The result is a goat that can produce the protein for spider silk in its milk. [1]
How is the silk extracted?
In an article written by T. Miller [1], she interviews Justin A., who helped create the original herd of these spider goats, and he explains how the silk is extracted from the goat’s milk.
Firstly, the goat’s milk is collected and frozen. Once the milk has thawed, it can be purified. The first step is to remove any fats and then filter out the smaller proteins. The spider silk protein is separated by selective precipitation (separating a solid from a solution [2]) and washed. Once a purified form of the spider silk protein is obtained, it is suspended in water and placed in a microwave. The purified liquid silk protein can be easily manipulated into its desired form.
THE AMAZING SPIDER GOAT (a short comic)
Spider Silk
Its structure and properties
The type of spider silk focused on by most studies is dragline silk. It has some interesting properties, such as having a good balance between strength and elasticity to enable the spider to catch flying prey. These unique properties means that it surpasses the majority of all natural and man-made materials [3].
Some of its most beneficial properties [3]:
- Strong
- Tough
- Biocompatible (compatible with living tissue [4])
- Minimally immunogenic (produces an initial immune response, but there are no long term effects)
- Exceptional cytocompatibility (has very little effect on the structure and function of tissues it comes into contact with [5])
- Slow degradation rate
Did you know? Spider silk produced by transgenic silk worms has been found to be 6 times tougher than Kevlar, which is used in bullet proof vests! [6]
These properties are a result of mainly two spidroins (proteins) that comprise the silk: MaSp1 and MaSp2. These proteins have very repetitive amino acid sequences that lead to the formation of specific final structures that give the silk its unique physical properties.[3]
Potential medical uses of spider silk
The use of spider silk in medicine is certainly not a new idea. In fact, it was even used by the ancient Greeks and Romans to promote wound healing [3]!
The possibilities for the biomedical applications of spider silk is what particularly interests me about this topic, since it relates to the majority of the modules I am currently studying. For example, both this module and the Orthopaedic Biomechanics module have covered tissue engineering and spider silk has shown great promise to enhance current solutions in this area [7]:
- Skin regeneration and wound dressing
- It has been shown to promote the healing of burns
- Cartilage and tendon tissue engineering
- Acts as a good scaffold because it degrades relatively slowly and scaffold shouldn’t degrade faster than the rate of new tissue formation [3]. It is also very biocompatible.
- Neural tissue engineering
- Has been proven to aid in nerve regeneration
Spider silk also has desirable properties for use in drug delivery and its high tensile strength and excellent biocompatibility make it a good choice for a suture [7].
Why not just use spiders?
- The spiders are very territorial, so are difficult to keep [3]
- The silk needs to be made in large quantities to be useful
Ethical concerns
As much as I see a great potential in the use of spider silk to improve healthcare, I understand that there are ethical concerns surrounding the use of transgenic animals. The procedures the animals go through are invasive (e.g. superovulation and taking tissue samples). It is also felt by some people that altering animals in this way is disrupting the natural order of the universe. Ultimately, it is important we take into account the welfare of animals when doing this type of research.
References
[1] T. Miller, “The Spectacular Spider Goat – Goat Journal,” Goat Journal, Aug. 12, 2021. https://goatjournal.iamcountryside.com/kids-corner/the-spectacular-spider-goats/ (accessed Mar. 23, 2025).
[2] “Selective Precipitation — Overview & Examples,” expii. https://www.expii.com/t/selective-precipitation-overview-examples-8536 (accessed Mar. 24, 2025).
[3] F. Bergmann, S. Stadlmayr, F. Millesi, M. Zeitlinger, A. Naghilou, and C. Radtke, “The properties of native Trichonephila dragline silk and its biomedical applications,” Biomaterials Advances, vol. 140, p. 213089, Sep. 2022, doi: https://doi.org/10.1016/j.bioadv.2022.213089.
[4] Merriam-Webster, “Definition of BIOCOMPATIBILITY,” Merriam-webster.com, 2017. https://www.merriam-webster.com/dictionary/biocompatibility (accessed Mar. 23, 2025).
[5] M. F. Sigot-Luizard and R. Warocquier-Clerout, “In Vitro Cytocompatibility Tests,” Test Procedures for the Blood Compatibility of Biomaterials, pp. 569–594, 1993, doi: https://doi.org/10.1007/978-94-011-1640-4_48.
[6] Bronwyn Thompson, “Bionic silkworms with spider genes spin fibers 6x tougher than Kevlar,” New Atlas, Sep. 21, 2023. https://newatlas.com/materials/silkworms-spider-genes-spin-fibers/ (accessed Mar. 23, 2025).
[7] B. Bakhshandeh, S. S. Nateghi, M. M. Gazani, Z. Dehghani, and F. Mohammadzadeh, “A review on advances in the applications of spider silk in biomedical issues,” International Journal of Biological Macromolecules, vol. 192, pp. 258–271, Dec. 2021, doi: https://doi.org/10.1016/j.ijbiomac.2021.09.201.
This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…