Press a button, print an organ. Perhaps the idea is not as Sci-Fi as it sounds. 3D bioprinting is an advancing field that uses layer-by-layer positioning of cells and biomaterials to produce living scaffolds for a variety of uses.
Depending on the qualities needed in the final product, techniques and materials vary. All start with a digital 3D model produced using computer aided design (CAD) software. One powerful feature of this is that CT and MRI scan data from patient can be used to tailor, for an example a tracheal graft, to personalised dimensions.
Next, the structure can be bioprinted using a bioink. Things to consider when choosing a bioink are the cells, biomaterial and growth factors included. Biomaterials such as alginate and polyvinyl-alcohol provide a structural scaffold for new cells to grow on. The ideal biomaterial must be biocompatible (not trigger an immune response) and biodegrade at the same rate as the new tissue grows.
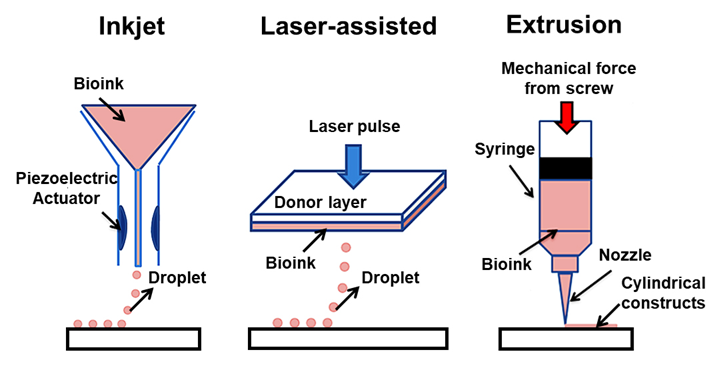
Cells and growth factors goes hand in hand, to print a bone graft you would use mesenchymal stem cells and a corresponding growth factor or chemical that encourages the pathway of differentiation looked for. The bioink used can dictate the printing method. Three popular approaches include inkjet-based, laser assisted and extrusion-based bioprinting. Each has their own set of opportunities and challenges.
Inkjet
Droplets of bioink, generated either through heating or a piezoelectric effect, are deposited on the substrate. High throughput, high resolution, low expense and strong cell viability count in favour of this technique. The key drawback is the need for low viscosity bioink to pass through the fine nozzle which results in low structural quality.
Extrusion
If a strong structure is a priority then extrusion printing comes to the fore. It relies on pneumatic or mechanical force to print uninterrupted lines of a far more viscous bioink. However, the increased shear stress involved reduces cell viability. High viscosity bioinks tends to result in lower resolution and the process is much slower.
Laser assisted
This uses a laser induced forward transfer technique (LIFT) which means that a laser is used to force material from a thin donor layer of bioink onto the substrate being printed onto. Advantages of this include high cell viability as there is no direct contact between the bioink and the dispenser so no stress forces and that the technique is compatible with a wide range of bioink of varying viscosities. Unfortunately, the complexity of this method results in high equipment cost.
Potential Uses
- Organ replacement
- Tissue grafts such as skin, bone muscle and cartilage
- Organs on a chip – used for drug and vaccination screening
- Drug delivery scaffolds
- Building disease models
Moving Forward
Printing organs for those currently awaiting a donor remains science fiction for now but great progress is being made towards that goal. However, even this is just the start as ethical considerations need to be made.
Integral to the whole process are stem cells and their source. The ethics of stem cells use are hotly debated but the alternative, induced pluripotent stem cells, are associated with more unpredictable behaviour.
Safety and quality control of bioprinted organs need to be considered, and this is made harder personalisation of treatment which reduces replicability of results. Arguably, for a terminally ill patient the benefits of an untested treatment outweigh the risk, but can this then be applied to non-life-threatening cases?
This is a well-structured and researched blog. The narrative demonstrates that the author is clearly interested by this topic but would benefit from more personal reflection throughout. What first made you interested in this topic? Why do you personally find it exciting? Do you think it is feasible? what are your opinions on the ethical considerations?