Growing up I spent a lot of time with my nan – something I always noticed was a faint ‘tick, tick, tick…’ coming from her. As I became older, she explained to me this was because she’d had some big surgeries and part of her heart was now made of metal (we used to joke that she was like iron man or the terminator). Her heart valves had become leaky, meaning they had to be replaced with mechanical valves in an open-heart surgery at Southampton General hospital. Because of my nan, I’ve always had a personal interest in how we use prosthetics in the heart.
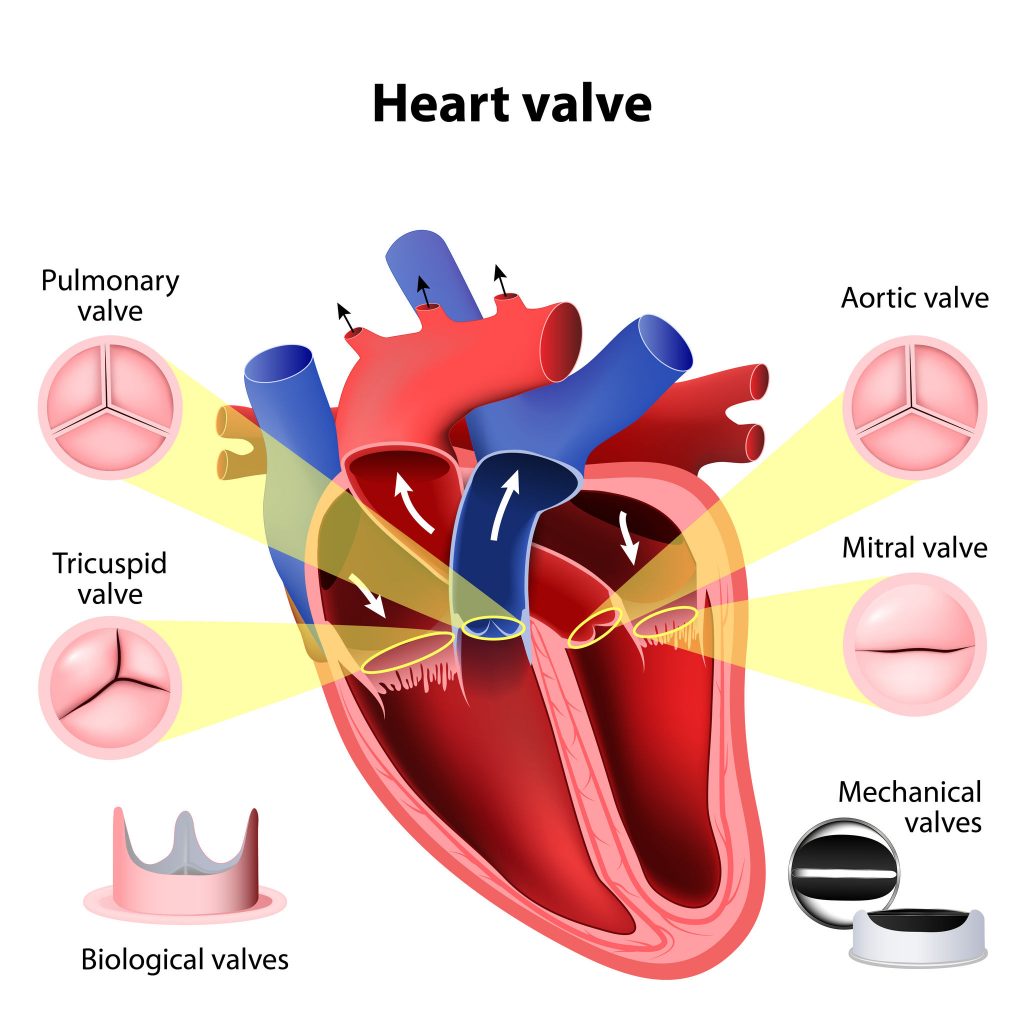
Prior to the surgery, my nan was given the choice between mechanical or biological valves, each with their own pros and cons. Biological valves typically last 10-15 years while mechanical valves can last a lifetime, making mechanical the go-to for patients under 65. Her team opted for mechanical valves so she wouldn’t need yet another risky open-heart surgery later down the line. 1
Figure 1: Diagram of the heart valves, alongside biological and mechanical valve replacements.2
Biological 0 – Mechanical 1
Despite this clear win for mechanical valves, they come with a major drawback – being prone to causing blood clots, which could lead to heart attacks or strokes. As such, patients with mechanical heart valves must take anticoagulants for the rest of their lives.
For my nan, this meant she had to take warfarin and required blood testing (by INR) every week to maintain the right ‘thickness’ of blood – too thick and you risk blood clots, too thin and you risk uncontrollable bleeding.4
Biological 1 – Mechanical 1
Biological valves not needing anticoagulation is an obvious score, however, there’s issues with xenotransplantation to consider. The majority of valves come from pigs or cows, meaning concerns are raised for animal welfare. To ensure the animal is healthy enough to provide a ‘safe’ transplant, they must be kept in sterile and confined laboratory conditions. In some ways this may be better than the conditions livestock have, but it’s still lacking for the animal’s nature. Having ‘good ethics’ is absolutely a requirement here.5
Biological 1 – Mechanical 2
The future of prosthetic heart valves
These are only a few of the positives and negatives for each traditional type of heart valve. It’s a complex decision and will depend entirely on the patient. However, in the time since my nan got her valves replaced, science and medicine has advanced. Open-heart surgery is still the norm for valve replacement, but transcatheter aortic valve implantation (TAVI) can now be used to avoid the obvious risks of open-heart surgery.
Another development is tissue engineered heart valves. This involves taking a scaffold which is seeded with stem cells and then then grown in a bioreactor before implantation. This would avoid the hazards associated with anticoagulation for mechanical valves, and the ethical issues of animal biological valves – and could grow along with the development in paediatric patients. Tissue engineered valves have not yet reached the clinical trials stage, but research is developing every day.8
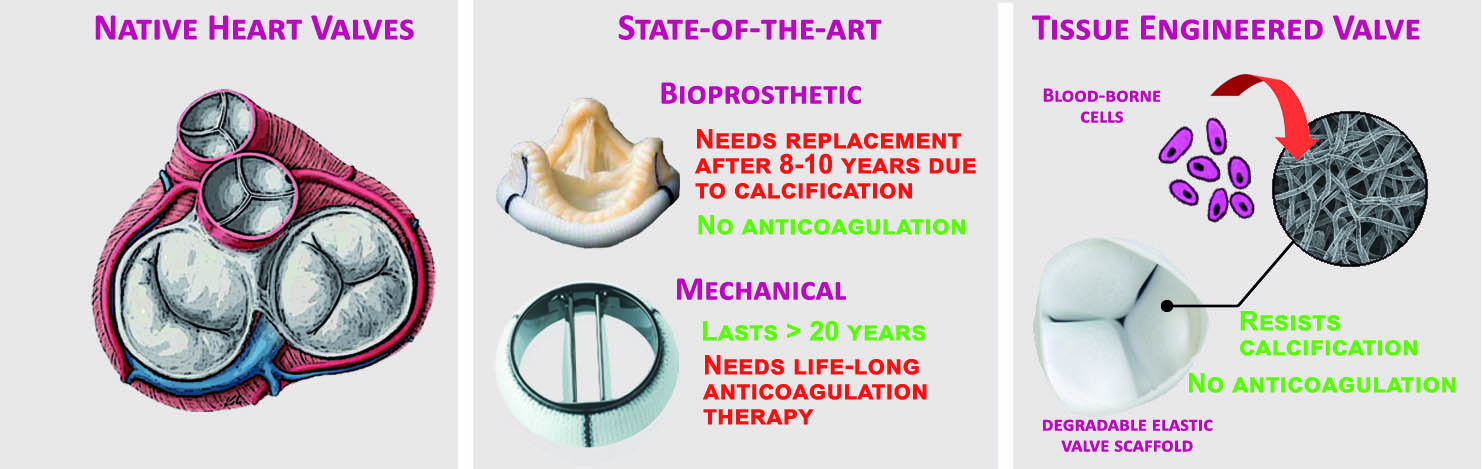
Figure 5: Comparison between native, biological, mechanical and tissue engineered heart valves9
With the heart being such an important organ, any improvements to the current procedures for replacement heart valve prosthetics are hugely beneficial. I’ve loved finding out more about how research is advancing in an ever-present field in mine and my family’s lives. One day I might be telling the future generations about how scientists grew new heart valves in a lab for me!
References:
- BHF. How do replacement heart valves work?, <https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/replacement-heart-valves> (2019). ↩︎
- Image source: https://heartsurgeryinfo.com/types-mechanical-heart-valves/ ↩︎
- Video source: https://youtu.be/hmU7UtzxowU ↩︎
- Catterall, F., Ames, P. R. & Isles, C. Warfarin in patients with mechanical heart valves. BMJ 371, m3956 (2020). https://doi.org/10.1136/bmj.m3956 ↩︎
- Rollin, B. E. Ethical and Societal Issues Occasioned by Xenotransplantation. Animals (Basel) 10(2020). https://doi.org/10.3390/ani10091695 ↩︎
- Video source: https://youtu.be/ojW7wZRF7Cg ↩︎
- Video source: https://youtu.be/q6erYCbZGMQ ↩︎
- Mendelson, K. & Schoen, F. J. Heart valve tissue engineering: concepts, approaches, progress, and challenges. Ann Biomed Eng 34, 1799-1819 (2006). https://doi.org/10.1007/s10439-006-9163-z ↩︎
- Image source: https://mirm-pitt.net/tehvalve/ ↩︎