There are many accidents and events that lead to pain and suffering, but none greater than the minutes following stubbing your big toe on the corner of a coffee table (disclaimer – this is not fact, purely for comedic purposes).
However, severe pain in the Hallux (a fancy scientific name for ‘big toe’) is an every day reality for many. 1 in 40 people over the age of 50 suffer from big toe arthritis (Hallux Rigidus) and 16% of those suffering foot pain identified the Hallux as the centre of pain.
Potential treatments
Solutions for Hallux pain date back to the Egyptians, where replacements toes were found from about 1000 BC and in recent years, it has been favourable to fuse the bones at the affected joint, limiting pain and consequentially movement. But, focus has recently shifted, due to revolutionising joint replacement technologies, prioritising the maintenance of as much bone and cartilage as safe and viable.

One example of this is Anika – a global joint preservation company, that is leading efforts to help people suffering from Hallux pain, particularly through their ToeMotion® and Toe HemiCAP® DF products. The video below providing an explanation of how this technology works (posted by Mason City Clinic).
Bones joint damage near toes can become debilitating and painful but relief is easier than you think. Osteoarthritis causes the bone and cartilage of the metatarsal the longest bone of the toe to wear down over time this causes pain and limits the toes effective range of motion. In more advanced cases both sides of the toe joint are damaged and a total resurfacing with implants on both sides of the joint may be necessary. The arthro surface toe motion total toe system is a simple procedure that can significantly reduce your pain while providing motion for a more active lifestyle. Here’s how it works. First your surgeon will insert a metal guide wire into the metatarsal bone ensuring that the implant itself will be inserted at exactly the right angle. Next the surgeon inserts a tapered screw designed for maximum strength, durability and fixation. Using a system unique to artho surface, the search and map several data points on your joint surface to figure out the curves of your damaged joint, ensuring that the implant will be a perfect fit. The surgeon then prepares the surface by means of a specialized reamer smoothing out the roughness caused by osteoarthritis and preparing the bone for the implant. Before placing the final implant on the metatarsal side, your surgeon will prepare the opposite side of the joint known as the phalangeal side similar to the technique for the metatarsal bone. The surgeon will begin by placing a metal guide wire, ensuring that the implant is inserted with the correct orientation. After shaping and preparing the bone for the implant, a metal base plate is screwed into place. The appropriate plastic implant is then locked into the base plate with the correct curve in thickness to match your joint. The phalangeal side implant is shaped like a cup and is designed to meet with the rounded metal implant on the metatarsal side. Once the plastic component is secured in place on the phalangeal side of the joint, the final metal implant is then locked into the screw on the metatarsal side, which completes the implantation. The final hem II cap implants are small, unobtrusive, strong and the only implants that have
screw fixation on both sides of the joint. The implants are designed to match variations in patient anatomy so the surgeon can obtain a personalized fit at the time of surgery. With the procedure
completed, the two sides of the joint moved smoothly against one another, simulating the movement of a toe joint. The toe motion procedure can be performed as an outpatient procedure, it’s minimally invasive, restores mobility and lets you enjoy an active lifestyle again.
Arthroplasty over Arthrodesis?
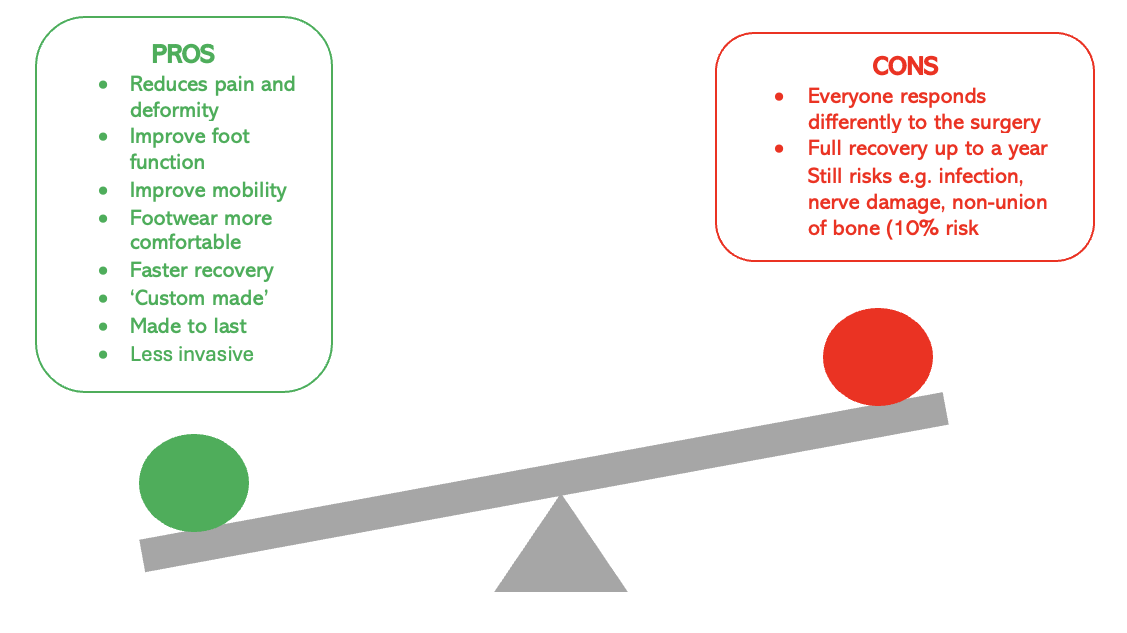
There are many arguments for why Arthroplasty is becoming more favourable than traditional Arthrodesis fusion methods (listed below), all of which are focused towards improving the patients care, recovery and experience with a toe joint replacement.

These arguments are supported by the successes of this medical advancement, which has helped people, at all levels, to get back on their feet. Furthermore, this technology is in line with the NICE joint replacement standards and actually seems to enhance them by giving patients more treatment options, preventing implant errors by removing less bone matter and improving rehabilitation with shorter recovery times.
Anna Lynch’s story: Anna feared she may never be able to walk pain free again, due to debilitating pain in her left big toe, but just months after her operation she trekked 10,000 feet up the Himalayas.
https://www.northeastfootandanklesurgery.co.uk/in-the-news.html
Despite overwhelming success, there is also still some drawbacks to this technology. For example it is fairly modern, so long term survival of the prosthetic cannot yet be disclosed with complete confidence and there is still lasting support for fusion as the more ‘reliable’ method of treatment. However, the benefits greatly outweigh the drawbacks (shown below).
Could this be BIGGER than the BIG toe?
There is also possibility to further this technology. Arthritis is now one of many disorders Hallux Arthroplasty can treat. Others include Hallux Vaglus (bunions), Osteonecrosis and unstable/painful MTP joints – making it a versatile treatment worth investing in.
The practises involved in this treatment have also been expanded to other areas of the body in hopes of achieving the same success, especially in places proven difficult to treat, such as the spine. This makes clear the significance of toe joint replacement technology and how the ideas and structures, e.g. replacement over fusion (shown in the image below), behind it, could revolutionise treatment for more difficult injuries, to allow greater movement and therefore quality of life for patients.

Right image from Mathur S, Jenis LG, An HS: Surgical Management of Chronic Low Back Pain: Arthrodesis, in Jenis LG, ed: Low Back Pain: Monograph Series
Left image from Jenis LG: Surgical Management of Chronic Low Back Pain: Alternatives to Arthrodesis, in Jenis LG, ed: Low Back Pain: Monograph Series. Rosemont, IL, Amer Acad of Orthop Surg, 2005.
My thoughts…
Overall, it could be considered that there is BIG potential for this shift from fusion to joint replacement technology to help improve patient care and quality of life. Starting by improving motion of the BIG toe and hopefully towards future success in more complex regions and functions.