POV: you donate your body to science and end up plastinated, posed like a ballet dancer, and touring the world in a glass box.

© Gunther von Hagens’ BODY WORLDS, Institute for Plastination, Heidelberg, Germany. Photo: Ines Huber.
www.bodyworlds.com
A Slightly Macabre Icebreaker
That’s (somewhat) the reality behind Body Worlds, the infamous exhibition created in 1995 by German anatomist Gunther von Hagens. Using plastination, a preservation technique he developed, von Hagens turned hundreds of real human bodies into anatomical art and took them on a global tour. Some call it groundbreaking. Others call it morbid, exploitative, or just plain weird.
From live autopsies on British telly to turning dead couples into NSFW dioramas, von Hagens hasn’t just flirted with controversy – he bought it dinner, dissected it, and stuck it under a spotlight like a 3 AM kebab.
Looks brilliant when you’re half-cut, but by morning? Bit dodgy, slightly greasy, and you’re left wondering what exactly you signed up for.
I first came across Body Worlds on social media. It creeped me out – but I couldn’t look away.
Not Just Skeletons in the Closet
Dead bodies might seem like a grim teaching tool, but they’re vital to modern medicine. Cadavers enable the understanding of human anatomy in 3D, not just in diagrams. No model can replicate the complexity, texture, or sheer messiness of a real human body.
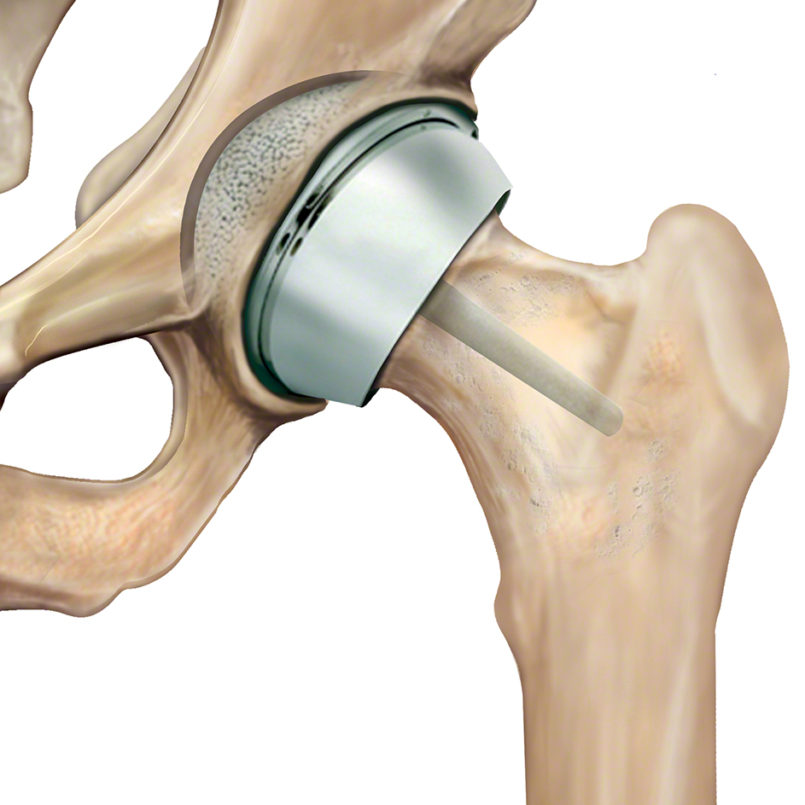
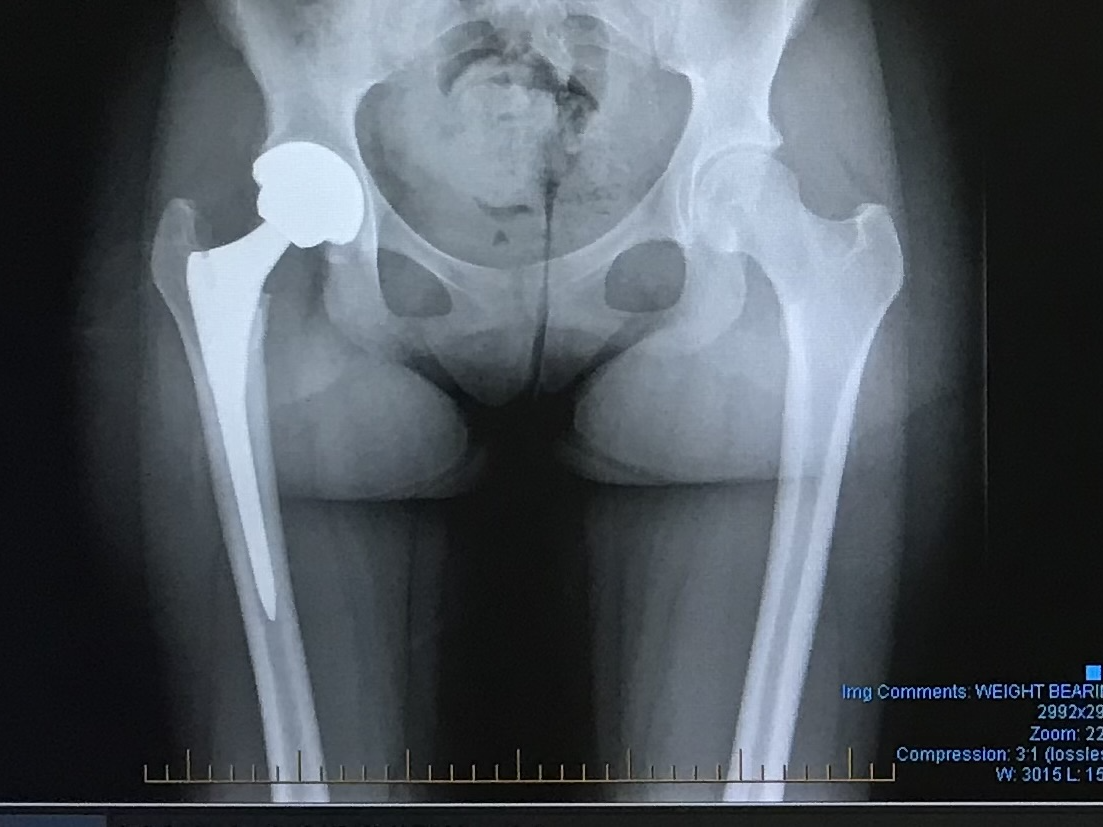
And for bioengineers? That mess matters. Whether you’re designing hip implants or bionic limbs, you need to understand what you’re replacing. You can’t replicate function if you don’t get form. Sometimes, death is the best teacher.

The von Hagens Dissection
(Metaphorically Speaking)
Von Hagens didn’t exactly ease into the public eye. Body Worlds toured globally with plastinated bodies posed in athletic stances, or intimate embraces. At one point, he even proposed plastinating a terminally ill donor for a “futurehuman” exhibit. (Yes, really.)
The ethical backlash? Instantaneous. In 2002, von Hagens performed the UK’s first public autopsy in 170 years.
Officials said it might be illegal.
The audience called it educational.
The media? Lost their collective minds.
Supporters argue Body Worlds promotes public education about the human body, health, and mortality. But that defence wears thin when you’re staring at a peeled-back corpse posed mid-basketball dunk.
Consent, Law & Ethics
The real ethical elephant? Consent.
Von Hagens has long insisted all bodies used in Body Worlds were donated willingly. But things got murky in 2002, when he returned seven bodies to China after fears they belonged to executed prisoners. He wasn’t charged, but the damage was done and whispers around sourcing have never really gone away.
In the UK, the Human Tissue Act 2004 governs the law on human remains: consent must be informed, documented, and respected. But globally? Standards vary. Some places are… less rigorous.
Even if it’s legal, is it moral? Does consent still stand when the final product ends up as ticketed entertainment?
Personal Reflection
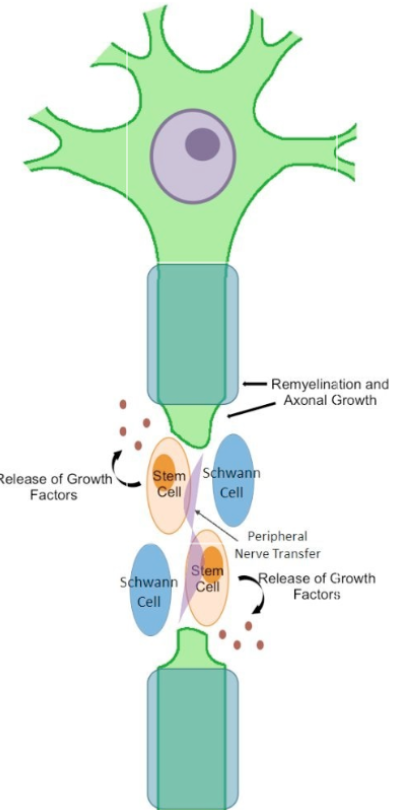
I already knew cadavers raised ethical questions, but this module sharpened that awareness. Exploring tissue engineering and body part replacement really highlighted how complex consent and anatomical use can be.
Do I think Body Worlds is cool? Yes. A bit much? Also yes. It walks a tightrope between science and spectacle… and sometimes jumps straight off.
Plastination sits uncomfortably between education and entertainment. At best, it teaches anatomy in a powerful, visual way. At worst, it commodifies it, teetering on disrepect.
In a world where our bodies become museum exhibits, how much say do we really have after death?
Literature
- Bohannon, J. (2003) ‘Plastination: putting a stopper in death’, Science, 301(5637), pp. 1173–1173. Available at: https://doi.org/10.1126/science.301.5637.1173.
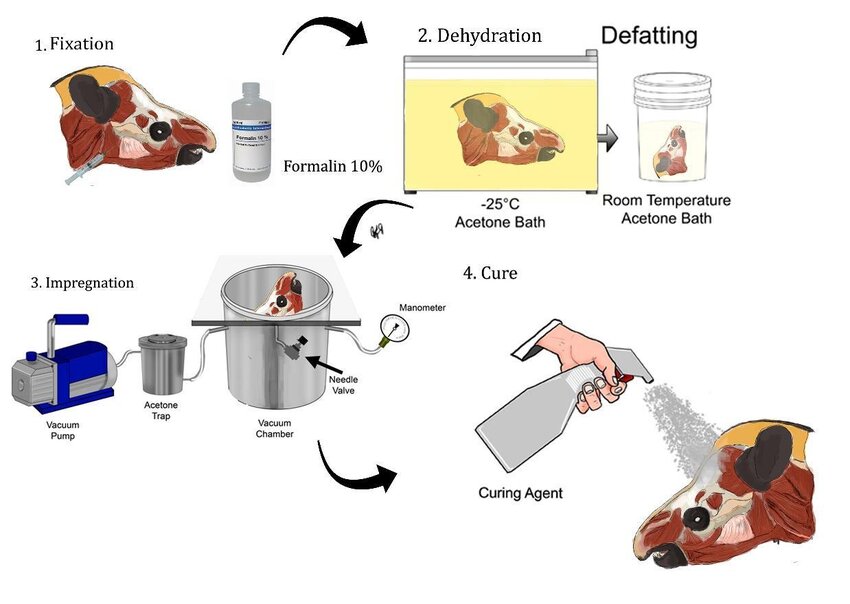
- Silva, M.V.F., Monteiro, Y.F., Miranda, R.P., Santos, A.B.D., Bittencourt, A.P.S.V., Carretta Júnior, M., Menezes, F.V., Delpupo, F.V.B. and Bittencourt, A.S. (2024) ‘From highways to biological collections: plastination of wild animals victims of roadkill in the sooretama biological reserve, brazil’, Brazilian Archives of Biology and Technology, 67, p. e24230044. Available at: https://doi.org/10.1590/1678-4324-2024230044.
- Tuffs, A. (2003) ‘Von Hagens faces investigation over use of bodies without consent’, BMJ, 327(7423), pp. 1068-c–0. Available at: https://doi.org/10.1136/bmj.327.7423.1068-c.






Leave a Reply
You must be logged in to post a comment.