Blog audio transcript:
Following the anatomy lab visit and lectures on stem cells, tissue engineering and prosthetics, it made me think about how far we can go towards developing an organ from a non-human origin. The heart stood out as one that could be in the realms of possibility compared to some of the more complex organs.
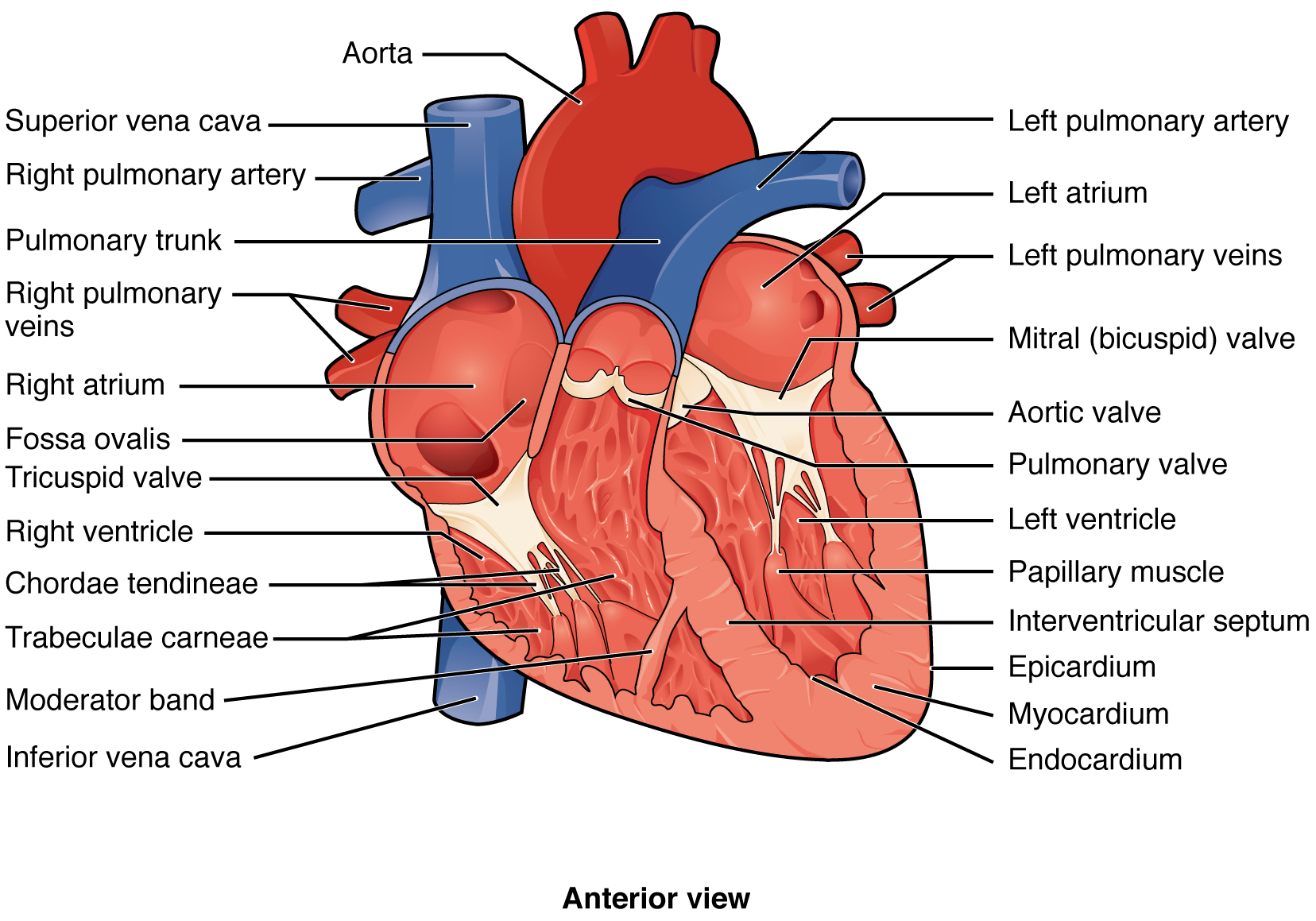
Genetically modified pig heart transplants have been carried out, with the first transplant performed in 2022 on a 57-year-old individual with end stage heart failure. This operation, formally called xenotransplantation, worked well for seven weeks, however the patient passed with heart failure after this time. It was found that the heart was vulnerable to rejection, it also contained traces of a virus that infects pigs.
There is a very good reflective article linked here which talks about where to go after this xenotransplantation was carried out. Feel free to have a look if you are interested in reading more.
This transplant brings up ethical points to consider along with scientific challenges:
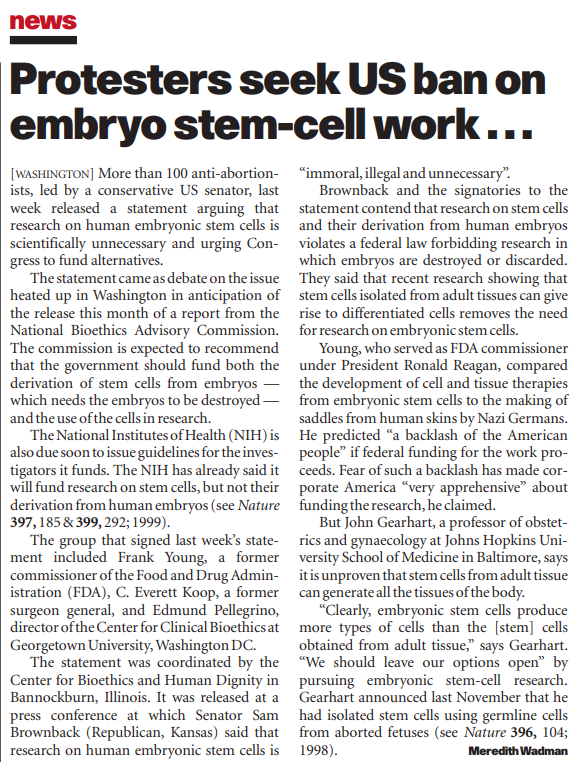
- To what extent is it right to sacrifice animals for the benefit of humankind? Applying ethical concepts, most people would say more good is done by saving a human life than by sacrificing an animal such as a pig. Furthermore, if a pig could be genetically modified to become more humanised in the future, then perhaps more than one human life could be saved for each pig. Provided that the pig is well cared for during its lifetime, then this action of using its tissue would overall be deemed as “good” and the “right” action.
- Scientific problems can happen during any transplantation. Specifically for pig heart xenotransplantation, immediate and acute rejection of the tissue can be an issue. Thrombosis, blood clots, can also occur due to a haematological incompatibility.
This video summarises the scientific and ethical implications of xenotransplantation:
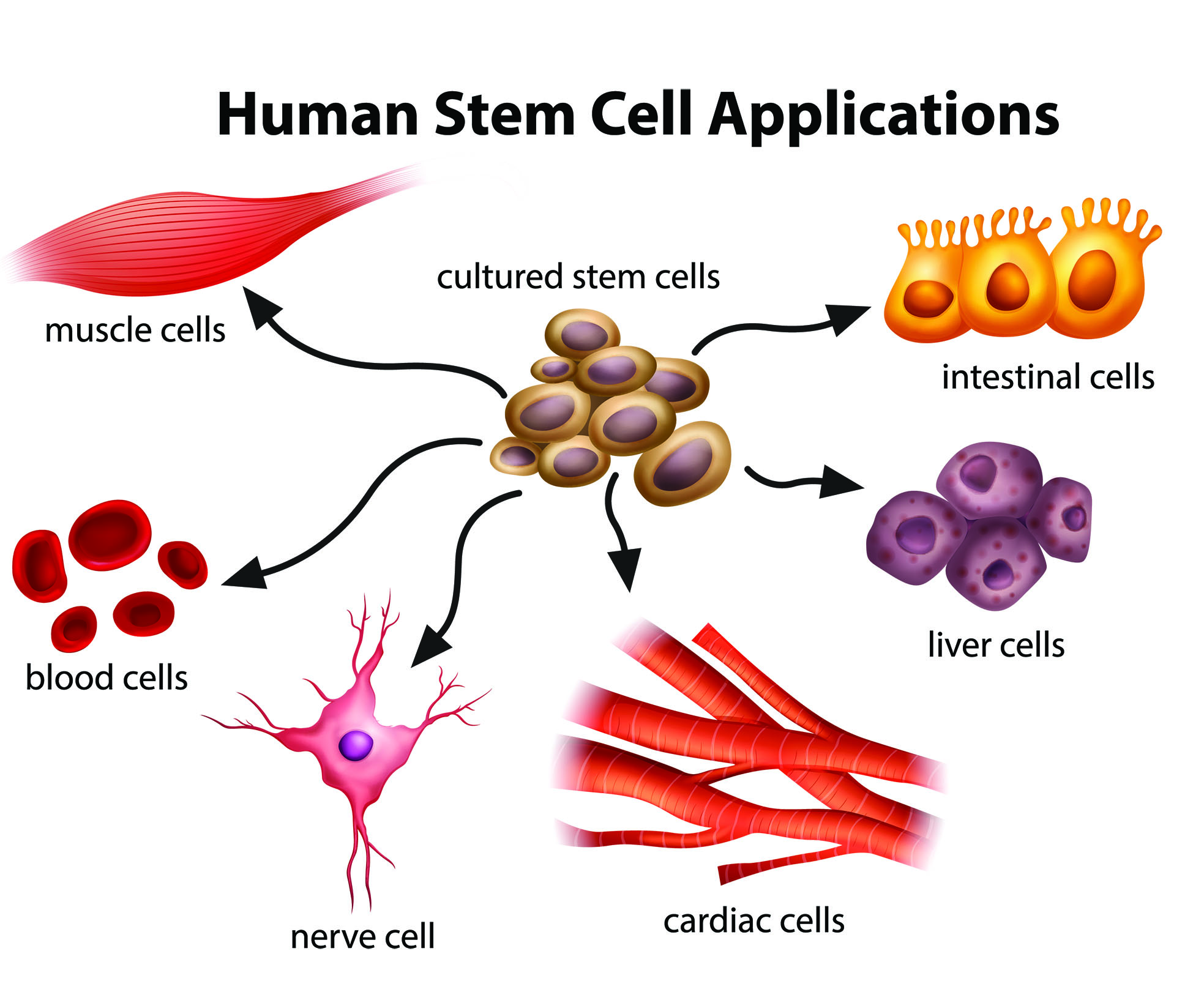
A recent BBC article published in January 2025 highlighted work done in Germany where stem cells were used to develop patches of heart muscle cells which were then grafted onto damaged tissue. This could help patients with heart failure, giving encouraging results in trials.

From a societal perspective, most of these developments on repairing heart tissue are novel. A high element of risk is not always worth it; however, it might be for those who have little or no alternative.
It is not uncommon to regularly come across news stories regarding the organ shortage. The UK organ donation law changed in May 2020 to an opt-out system meaning that by default adults are considered as potential donors.
In my view the moral status of a human life outweighs the sacrifice of an animal such as a pig. Scientific advance in this area should be encouraged within the framework of ethical boundaries. I cannot find a meaningful downside to pursue alternative methods of sourcing valuable organs.


This is a good blog. It nicely demonstrates a good understanding of organ-on-a-chip technology and clearly explains its purpose and…
This is a good blog, very engaging with a good backgroud to 3D bioprinting. You could improve your blog with…
This is a good, very interesting blog about necrobotics. It explores the idea of necrobiotics which is fairly new approach…
This is a good blog. You introduce the reader to the topic of prosthetics and bionic limbs in a very…
This is a good blog introducing hernia mesh benefits and drawbacks. You create a narrative in this blog, which showcase…