Cochlear implants have been an approved method of treatment for the profoundly, and more recently severely, deaf since the late 20th century. Their continued technological improvements since have provided those patients with the ability to hear through a processor (Hainarosie, 2014). The audio is not a perfect replication of natural hearing, but allows for interpretation of speech and sound in a way the brain can understand. Modern technology around cochlear implants provides patients with the option to have the external processor of their implant either behind their ear or off of their ear. Both designs allow for bluetooth connection between phone and processor, and each option has its own positives and negatives for users to consider.
Behind-the-ear (BTE) Cochlear Implants
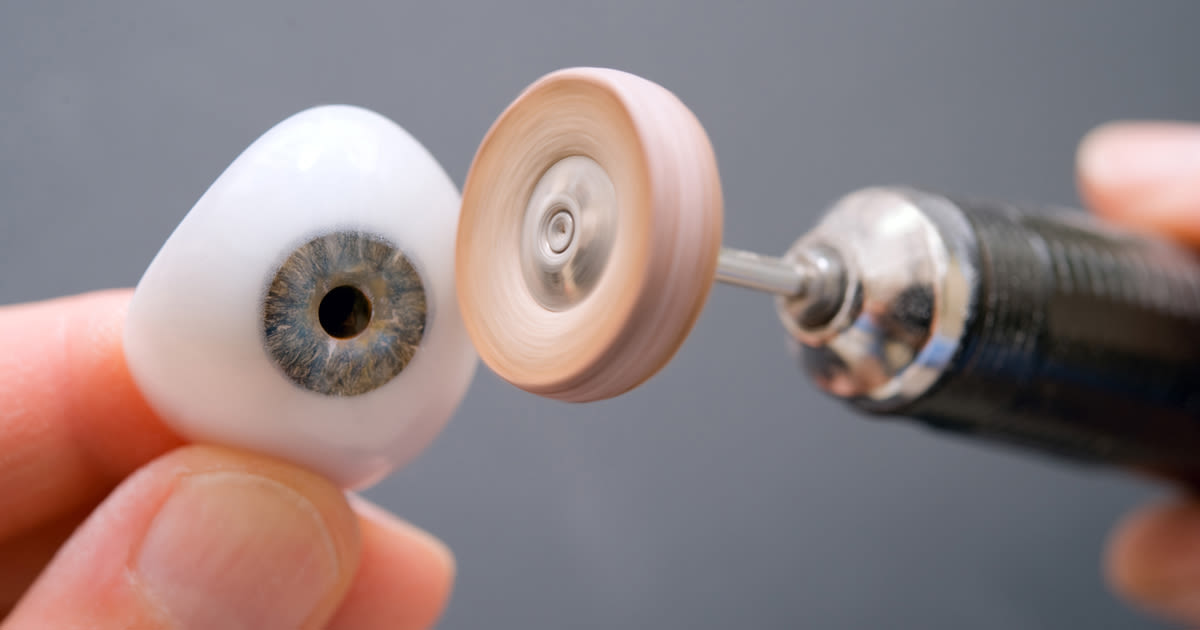
BTE cochlear implants are the originals – this design for the external processor has been used since implantation in the cochlear began. The processor (containing the microphone) sits on the ear of the user and a short cable connects this to the magnet that transfers the audio information to the electrodes implanted in the cochlear. The location of the microphone on these processors differs between companies. For example, Advanced Bionics’ Naida Cl M sound processor has the microphone dipping down into the outer ear region whereas Cochlear’s Nucleus 8 sound processor has dual microphones. Each company has taken a slightly different approach to the goal of reducing background noise and making the sound as close to natural hearing as possible.

BTE – Naida Cl M sound processor – Advanced Bionics

OTE – Kanso 2 sound processor – Cochlear
Off-the-ear (OTE) Cochlear Implants
OTE cochlear implants are a more recent development in cochlear implant technology with Cochlear’s Kanso 1 sound processor being released in 2016. These processors contain only one piece that sits on the side of the head connecting directly to the magnet inside the head. There is no part that rests on the ear. Because of this, some users find it more comfortable because their ear can have a break from holding the processor. However, it is often found that the magnet needs to be stronger to ensure that the processor does not fall off because it is a less secure connection. This is a problem for some people as they feel more comfortable with a processor on their ear when they are playing sport or in other situations where the processor could get dislodged. The single piece design of the OTE processor means that the microphone is placed on the side of the head. This can have some impact on the audio that the user receives as it is not being collected from the natural location – the outer ear.
Conclusion
Some cochlear implant users opt to obtain both a BTE and OTE sound processor after surgery so that they can use each to their strengths. Throughout reading for this blog I found that my preferred design is the Naida Cl M sound processor by Advanced Bionics because of its microphone location and BTE design. A BTE design allows for better microphone placement and a more secure feeling whilst an OTE design allows for a more discrete processor with fewer pieces attached to the head – perhaps making glasses or hat wearing slightly easier. To improve comfort around OTE sound processors, there are clips and headbands available. I think that it is important for each user to be able to weigh up the pros and cons of each processor type to make an informed decision about which would work best with their lifestyle. Perhaps the difference in age between two patients would be enough to result in different choices. Access to both processor types appears to be a great solution for those who find that OTE and BTE processors are each useful in different parts of their life.
Further reading suggestions:
A Reddit thread discussing personal experiences with OTE and BTE processors:
A list of current cochlear implant processors available in the UK:
https://www.bcig.org.uk/ci_manufacturers.aspx
Cochlear’s comparison of their current sound processors:
References:
Hainarosie, M., Zainea , V. and Hainarosie , R. (2014) ‘The evolution of cochlear implant technology and its clinical relevance’. Journal of Medicine and Life. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391344/ (Accessed: 8 March 2024).






Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…