Utilising stem cells in 3D printing technology has opened up a massive amount of potential in regenerative medicine and is rapidly improving. 3D printing using stem cells is being used today to revolutionise the food industry by providing an alternative to regular meat!
I believe the industry holds promise and can provide a highly customizable and slaughter free alternative to conventional meats. While also tackling issues like climate change, gas emissions and food waste.
What is 3D-printed meat?
It is a type of cultured or programmable meat replica made from the process of 3D printing using stem cells, attempting to mimic regular farmed meat at a cellular level. Aiming to recreate the taste, smell and texture of conventionally farmed meat.
How is 3D printed-cultured meat made?
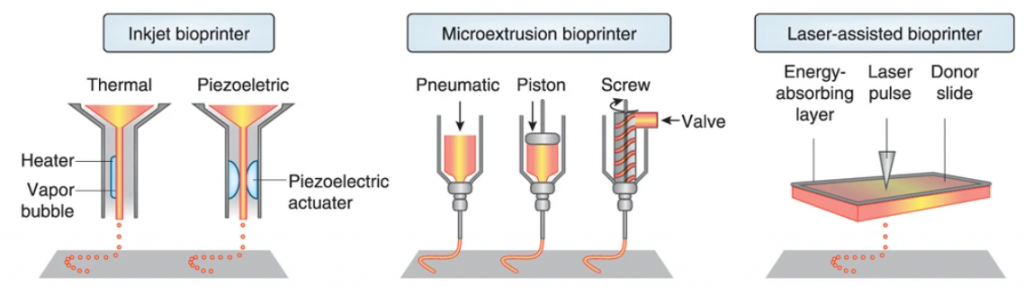
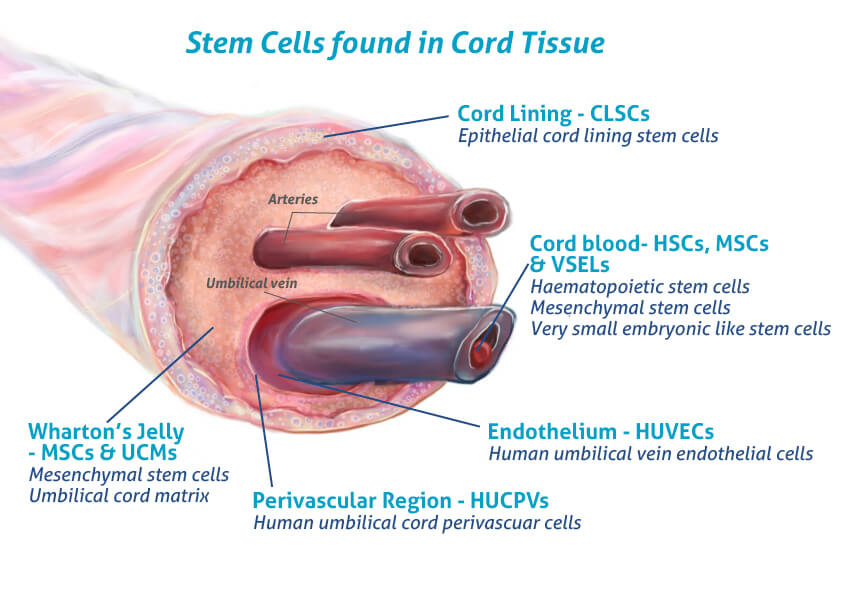
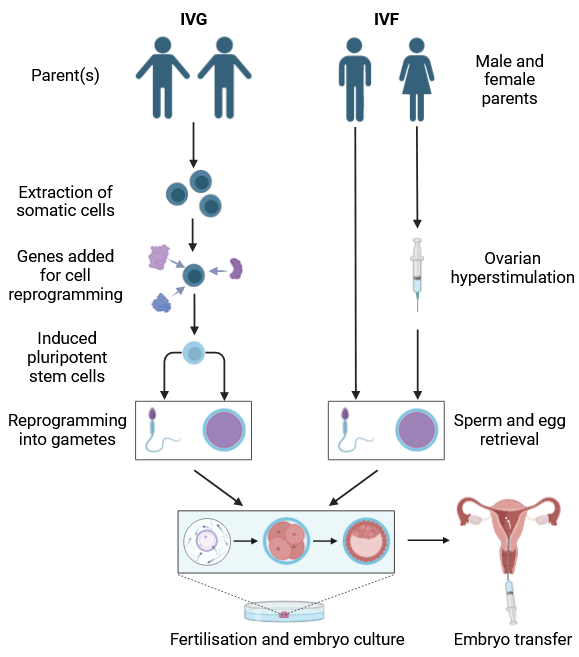
While production does require fat and muscle cells from an animal, no slaughtering of livestock is required. The process utilises stem cells that scientists choose depending on the type of meat desired. These cells then undergo a proliferation process, and are bathed in a nutrient dense serum in a climate-controlled bioreactor.

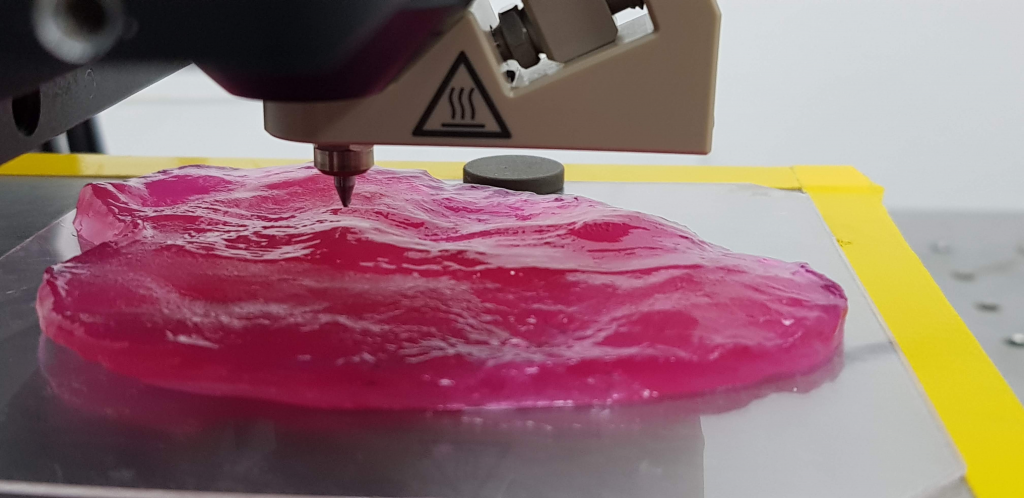
After several weeks the cells will differentiate into fat and muscle cells that form the bio-ink. A robotic arm with a nozzle dispenses the cultured meat filament crafting the meat layer by layer. The arm following instructions using a computer-aided design to form the intended structure.
The product is incubated again allowing the stem cells to further differentiate and mature, the muscle fibres once fully developed will have the right thickness, length and density and after a few more weeks the meat is ready to be cooked and served for consumption!
The video below shows how researchers at Osaka University utilised 3D printing with stem cells isolated from Japanese cattle to make wagyu steak :
Why stem cell-cultivated meat?
The food industry is resource intensive and needs large quantities of land and fresh water, With Our world in Data stating that “food production accounts for over a 1/4 of global greenhouses emissions”. By utilising 3D printing and cultured-meat harvests we can address the ethical concerns associated with animal farming, but also decrease agricultural land and water usage, leading to enhanced energy efficiency.
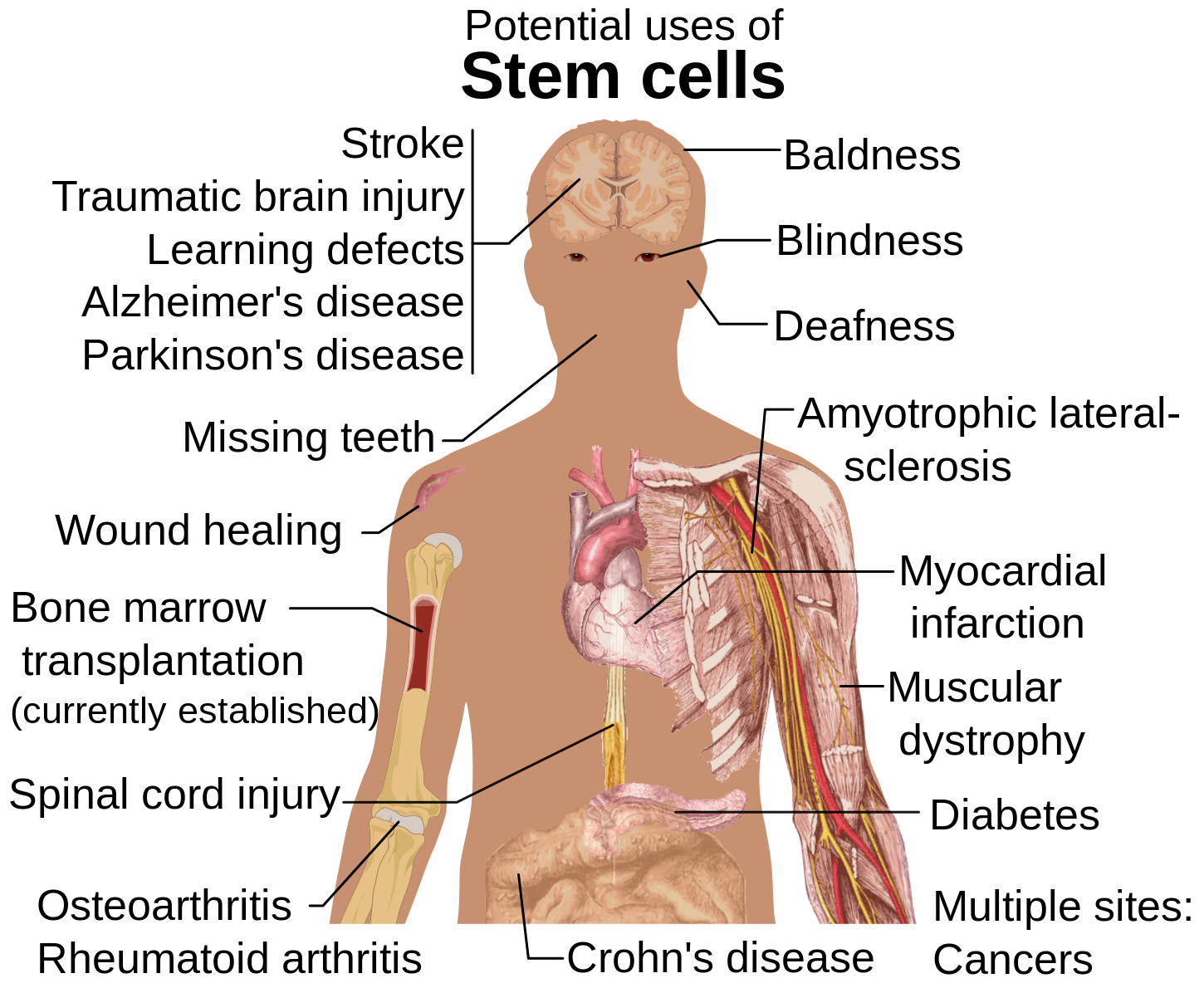
Stem cells are one of the most important cells for any organism due to their ability to turn into other types of cell, and are crucial in advancing the field of synthetic meats.
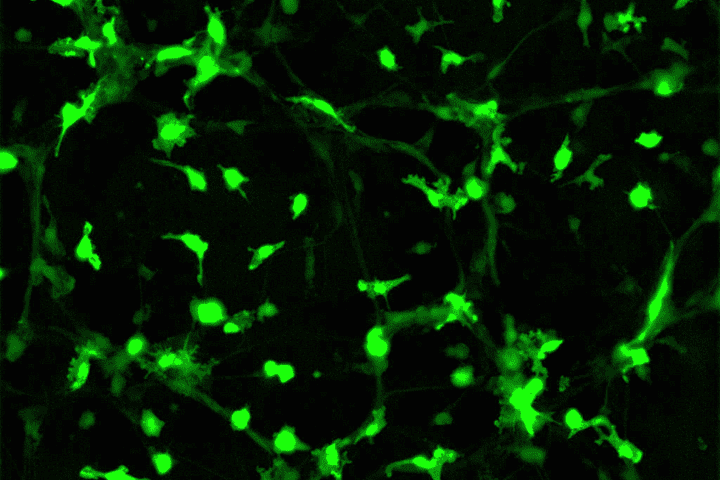
Professor Hojae Bae and his team at Konkuk university are using immortalised fibroblast cells implanted with two genes to transform them into muscle and fat-laden cells, aided by an optimised 3D-printable hydrogel scaffold to grow cells for printing steaks. The image displays the fat and muscle cells together with microchannels.

The future of 3D-printed meat ?
The cost to produce cultured meat was estimated to be about $700 per kilogram by a lab at Konkuk University, with the average cost of a 3D-food printer being between $1000-$5000 with additional costs for food-grading machines for meat production.
The procedural process can also be difficult, with varying qualities of meat and an entire tissue engineering stage prior to actual printing. The 3D printers specific for production of meat are also in need of further development, to ensure that the food manufacturing process is safe.
With the Singapore Food Agency accepting the world’s first cultivated chicken for sale in Dec 2022, it is only a matter of time before other nations follow. I believe that once these issues are attended to 3D-printed meat will soon play a pivotal role in challenging the environment and ethical issues regarding conventional farmed meat.







Very well written, with an excellent format and images. You’ve included interesting statistics and related it to personal ideas which…
This is a very well written blog, the format is as if you are talking directly to me. The ideas…
Love the Batman GIF :)
This is an excellent, well written blog. The narrative is engaging and easy to follow. It could be improved by…
This is a well-communicated blog. The it is written well with good use of multimedia. It could be improved with…